UPDATE March 2020: The Government have published their response to the final report.
October 2018: The inquiry published their final report. Download from inquiry web site.
- Download TMSA submission in PDF format
- Download other submissions from the Inquiry web page
- Dr. Mary Ackerley’s submission
MEDIA ARTICLES
- ABC article about mould, health effects and tenancy (15/8/18)
- Article about CIRS and the inquiry from The New Daily (17/8/18)
- Article about CIRS and inquiry from Buzzfeed (28/9/18)
- Article from Nine news about final report (17/10/18)
- Article about CIRS and inquiry from Buzzfeed (22/10/18)
- Article from HVAC&R News about the final report (25/10/18)
- ABC AM Radio segment (and article) about final report and mould illness (25/10/18)
- Follow up ABC AM Radio segment (and article) about tenants and mould (29/10/18)
- Article from The Fifth Estate about the final report (1/11/18)
- Article from Coast Community News about the final report (9/11/18)
- Article from Nine news about mould avoiders (10/11/18)
- Article from The Daily Telegraph about CIRS & Lucy Wicks (14/11/18)
To: The Standing Committee on Health, Aged Care and Sports
Inquiry into Biotoxin-related illnesses in Australia Submission
Date: 2 August 2018
Prepared by: Caleb Rudd on behalf of Toxic Mould Support Australia
Contents
Executive Summary
Introduction
Defining Biotoxin-related illnesses and Chronic Inflammatory Response Syndrome
Response to terms of reference
1. The prevalence and geographic distribution of biotoxin-related illnesses in Australia, particularly related to water-damaged buildings
2. The prevalence of Chronic Inflammatory Response Syndrome (CIRS) or biotoxin related illness in Australian patients and the treatment available to them
3. The current medical process of identifying biotoxin-related illness in patients and the medical evaluation of symptom complexes attributed to biotoxins and CIRS
4. Any intersection with other chronic diseases
5. Investment in contemporary Australian research to discover and provide evidence of CIRS as a chronic, multisystem disease &
6. Research into biotoxin-related illness caused from water damaged buildings
7. Any related matters
Conclusion
References
Executive Summary
- Toxic Mould Support Australia is a website and Facebook group that provides support and awareness for Australians suffering from CIRS-WDB and other mould related conditions.
- CIRS-WDB is a complex, multi-symptom, multisystem illness caused by exposure to biotoxins in water-damaged buildings. It is not mould allergy or mould infection.
- The prevalence of CIRS-WDB in the Australian population is unknown at present. A study in the United States estimated the prevalence of CIRS as being 7%.
- The World Health Organization estimates 10-50% of Australian buildings are affected by indoor dampness.
- CIRS-WDB and mycotoxins have been linked to a number of chronic health conditions including Chronic Fatigue Syndrome, Alzheimer’s disease, depression, Sarcoidosis, Multiple Chemical Sensitivity, and Autism Spectrum Disorder.
- Screening and diagnosis of CIRS-WDB can be done via symptoms, visual contrast testing and blood biomarkers. Accurate testing for many biomarkers is not available in Australia.
- There are relatively few general practitioners in Australia who are aware of CIRS and who can diagnose and treat the condition.
- Treatment medications are available in Australia but most medications must be compounded.
- CIRS-WDB patients need access to more CIRS aware health practitioners, diagnostic testing, and affordable medication.
- Funding into studies examining the prevalence of CIRS-WDB and water-damaged buildings, and clinical treatment studies, is urgently required.
- This submission outlines recommendations for increasing access and affordability of CIRS diagnosis and treatment. It also offers recommendations for the prevention of constructing water-damaged buildings and the testing and remediation of current ones.
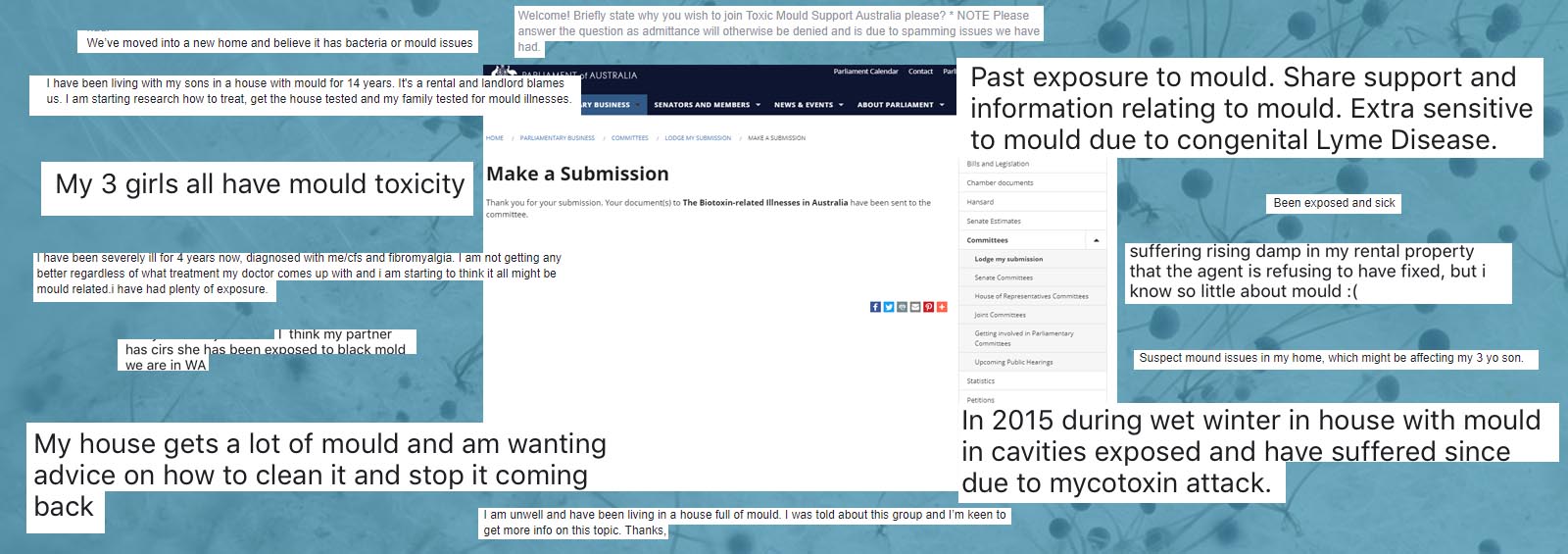
Toxic Mould Support Australia (TMSA) started as a Facebook group in October 2013 (Toxic Mould Support Australia Facebook Group, n.d.). TMSA expanded to include a website (Toxic Mould Support Australia, n.d.) in September 2015. As of August 1st 2018, the Facebook group has 3,285 members and the website has averaged 2,280 visitors per month over the two month period June-July 2018.
Daily, the administrators of the Facebook group voluntary provide support, education and awareness to individuals and the community as a whole about the effect of water-damaged buildings on health, particularly in regards to CIRS. Daily, we hear the heartbreaking stories of those afflicted with chronic illnesses related to mould and see photos of terrible water damage to buildings. People write about how CIRS has devastated not only their health, but their relationships, their finances, and their faith in the medical, welfare and legal systems of this country.
Note: Many TMSA members, due to the severity of their symptoms, are not well enough to write a submission for this inquiry.
Defining Biotoxin-related illnesses and Chronic Inflammatory Response Syndrome
CIRS is a complex, multisystem, multi-symptom illness due to exposure to biotoxins, inflammagens and toxicants in the environment that triggers a chronic pro-inflammatory innate immune response in humans.
CIRS-WDB is CIRS caused by the exposure to the interior environment of water-damaged buildings (WDB). There are causes of CIRS other than water-damaged buildings (outlined in response to terms of reference 4), however, CIRS-WDB is the main focus of the inquiry and this submission.
Biotoxins are toxins from biological sources. In the context of CIRS-WDB they include fungal spores, fungal cell and hyphal fragments, which are recognised as Pathogen-associated molecular pattern (PAMPS) by the immune system, mycotoxins, microbial volatile organic compounds (VOCs), building material VOCs, bacteria, bacterial endotoxins, protozoa, viruses, actinomycetes, beta glucans, mannans and more (World Health Organization Europe, 2009; Berndtson et al., 2016; Hope, 2013).
Biotoxin illness is an umbrella term for the various types of CIRS.
CIRS-WDB was a term coined by Dr. Ritchie Shoemaker in 2009 (Shoemaker, & Mazeil, 2009), first appearing in published peer review literature in 2013 (Shoemaker, House, & Ryan, 2013). Previously it was referred by Shoemaker and colleagues as Sick Building Syndrome (SBS) (Shoemaker, & House, 2006). Other researchers have also labelled CIRS-like conditions as SBS (Straus, 2011), especially in the Asia region (Takaoka, Suzuki, & Norbäck, 2016; Nakayama, & Morimoto, 2007). Other names include Dampness and Mold Hypersensitivity Syndrome (DMHS) (Valtonen, 2017; Daschner, 2016), mold-related illness (Tuuminen, & Sakari Rinne, 2017; Shenassa, Daskalakis, Liebhaber, Braubach, & Brown, 2007), Environmental Acquired Illness (EAI) (International Society for Environmentally Acquired Illness, n.d.), mold illness, toxic mold illness, mycotoxin illness and mycotoxicosis (Gray et al., 2003). The Global Indoor Health Network (GIHN) recently released a paper with over 400 references that summarised the nomenclature, diagnostic process and treatments for CIRS-like disorders (2018).
Regardless of the name they all describe similar syndromes or illnesses; chronic systemic conditions that go beyond allergy and respiratory issues, although they may include those as well. These other symptoms include fatigue, headache, immunological issues, flu-like symptoms, neurological issues, digestive problems/IBS, chemical sensitivity, exercise intolerance/PENE (post exercise neuroimmune exhaustion), and cognitive impairment. As with Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS) the risk of suicide compared to the healthy population is increased among CIRS patients.
CIRS-WDB is not allergy but rather an inflammatory illness caused by toxins inhaled via exposure to water-damaged buildings.
Response to Terms of Reference
1. The prevalence and geographic distribution of biotoxin-related illnesses in Australia, particularly related to water-damaged buildings:
The World Health Organization estimate of 10-50% of Australian buildings are affected by dampness (World Health Organization Europe, 2009, p93).
It is important to note that water damage and fungal growth is not always visible. Mould and bacterial growth can happen behind furniture or appliances and in wall cavities, ceilings and subfloors due to water ingress or build-up of condensation (Schwartz et al. 2016; ANSI/IICRC ii, 2015).
Berndtson et al. (2016), building upon the U.S. Government Accountability Office (2008, p7) case definition, defined the case definition for CIRS-WDB as the following:
- There must be the potential for exposure to a building with water damage and subsequent amplified microbial growth. Amplified growth is documented by any of the following: (i) the presence of visible mold; (ii) the detection of musty odours; or (iii) commercial testing which demonstrates amplified mold growth by species known to flourish on damp indoor building materials.
- There must be multiple symptoms involving multiple systems in a possible case of CIRS-WDB, similar to those seen in patients reported in peer-reviewed, published studies.
- There must be laboratory abnormalities in a possible case that are similar to those seen in peer-reviewed, published studies.
- There must be improvement with therapy similar to that reported in peer-reviewed, published studies.
Dr. Shoemaker and Australian mycologist David Lark conducted a study in 2016 using mould specific quantified PCR (QPCR), a type of DNA testing, of homes, workplaces and schools. In the study they used a scoring system called HERTSMI-2, that uses a scale from 0 (low fungi levels) to 50 (extreme fungi levels). When pooling samples from 807 buildings across Australia and the United States, they found the mean HERSTMI-2 score for homes was 17.6, workplaces was 15.5, and schools was 17.8. According to the same study, a CIRS patient needs a HERTSMI-2 score of 10 or less to prevent relapse (Shoemaker, & Lark, 2016).
2. The prevalence of Chronic Inflammatory Response Syndrome (CIRS) or biotoxin related illness in Australian patients and the treatment available to them:
Australia is lacking epidemiological data on the prevalence and incidence of CIRS in the Australian population.
The only prevalence data to date on CIRS in the United States comes from two studies lead by Dr. Scott McMahon. Retrospectively analysing 1061 patients at a CIRS speciality clinic then compared with 127 children presenting for wellness checks at a paediatric clinic (McMahon, Kundomal, Yangalasetty, 2017), he states:
“At a prevalence of ≥ 7.01%, chronic inflammatory response syndrome is one of the greatest public health dilemmas in existence.” (McMahon, 2017).
7% of the Australian population would amount to 1.73 million people in total based on a total population of 24,770,700 (Australian Bureau of Statistics, 2018).
There are only a few specialist general practitioners (GPs) who know how to screen, diagnose and treat CIRS-WDB in Australia, most of whom belong to the Australian Chronic Infectious and Inflammatory Disease Society (Australian Chronic Infectious & Inflammatory Disease Society, n.d.).
Treatments available for CIRS in Australia:
Treatment involves a step-wise treatment protocol developed by Dr. Ritchie Shoemaker that involves the following steps (abbreviated from Shoemaker et al., 2018):
- Removal from the biotoxin source. In CIRS-WDB this means remediation of the home and/or workplace. Often, due to the cost of remediation or extent of water damage, this is not possible so relocation is critical. This is also costly as it may include replacing of possessions due to avoiding cross-contamination of a new abode, if one can be found.
- Binding of biotoxins using medication, such as cholestyramine, a bile acid sequestrant.
- Treating of multiple antibiotic resistant coagulase negative staphylococci (MARCoNS) if present.
- Correction of inflammatory and hormonal dysregulation.
- Use of vasoactive intestinal polypeptide (VIP) spray to normalize hormonal abnormalities, inflammatory change and gene expression, and restore brain grey matter atrophy.
All of these treatment options are available to Australian citizens, however there are at least three barriers to treatment:
- The biggest hurdle for Australian patients is finding accommodation or work places that do not have water damage. See response to item 7 for more details.
- Cholestyramine is only available on the PBS as Questran-lite (Aspen Pharma Care), a medication that contains aspartame. Many CIRS patients have chemical sensitivities to aspartame and rely on the more costly additive free compounded version.
- Recommendation: An additive free version of cholestyramine or at least the previously available sugar version (also Aspen Pharma Care) be introduced to the Australia marketplace.
- Medications, including EDTA and colloidal silver nasal spray and VIP nasal spray, are only available as expensive compounded medications.
3. The current medical process of identifying biotoxin-related illness in patients and the medical evaluation of symptom complexes attributed to biotoxins and CIRS:
There are three methods of screening that can also be used as for diagnosis, currently in use by Australian CIRS aware health professionals.
- Symptom cluster analysis:
- Dr. Shoemaker has developed a symptom cluster table of 37 symptoms divided into 13 groups. If an adult patient has one or more symptoms in 8 or more clusters, the likelihood of CIRS exceeds 95%. For children, 6 or more clusters are indicative of CIRS (Shoemaker et al, 2018). If an adult patient is positive for 6-7 clusters, further testing may be warranted (Berry, 2014).
- Visual contrast sensitivity (VCS) testing:
- Due to increased inflammation and hypoperfusion in the optic nerve, visual contrast is typically reduced in CIRS. Done either with a handheld kit or an online version (Online VCS Screening Test, n.d.) a positive VCS coupled with a positive symptom cluster increases the screening accuracy to 98.5%, with a false negative rate of < 2% (Shoemaker et al., 2018).
- HLA DR/DQ genetic susceptibility:
- Via testing of over 10,000 patients, Dr. Shoemaker has identified genetic susceptibilities in HLA-DR and HLA-DQ haplotypes, interrelated groups of genes, that confer susceptibility for CIRS-WDB and other CIRS types (Lab tests for mold illness, n.d.; Gunn et al, 2016; Shoemaker et al. 2018). Dr. Shoemaker has described a susceptibility of 25% in the general population to CIRS-WDB (Shoemaker, 2010). While there have not been large scale studies published as yet, there is a growing number of studies showing susceptibility of HLA for autoimmune diseases. These include coeliac disease, rheumatoid arthritis, spondyloarthritis (Bodis, Toth, Schwarting, 2018) and sarcoidosis (Rossman et al., 2008). Also a portion of people vaccinated with the Lymerix vaccine developed Lyme arthritis with the same susceptible polymorphisms that Dr. Shoemaker found (Steere et al., 2006).This can be tested for in Australia using the Sonic Healthcare Ltd. group of pathology laboratories (HLA Panel Screen (DR and DQ), 2015).
Note: Methods 1 and 2 do not stratify between CIRS types. 3 can (to a limited extent).
If positive for one or more of the above tests, a confirmatory diagnosis involves measuring the following hormonal blood markers and growth factors (Shoemaker et al., 2018):
- alpha-Melanocyte stimulating hormone (MSH). Usually low. +
- Vascular endothelial growth factor (VEGF). Often low or high. +
- Antidiuretic Hormone (ADH) a.k.a. Vasopressin. Often low. *
- Vasoactive intestinal polypeptide (VIP). Often low. *
In addition measuring markers pro-inflammatory cytokine markers (standard inflammatory markers such as CRP and ESR, and IgE antibodies to mould, are usually not abnormal):
- Transforming growth factor beta-1 (TGF-b1). Often high. +
- Complement 4a (C4a). Often high. +
- Matrix metallopeptidase 9 (MMP-9). Often high. +
- Often high. *
+ Not available through a NATA/RCPA accredited Australian laboratory.
* Available through a NATA/RCPA accredited Australian laboratory.
Other tools such as volumetric brain MRI analysis using the FDA approved NeuroQuant software (Shoemaker, House, & Ryan, 2014) and testing for multiple antibiotic resistant coagulate negative staphylococci (MARCoNS) in the deep nasal passages can also aid in diagnosis and track treatment progress.
CIRS screening and diagnosis in Australia is hampered by the following factors at present:
- There are a limited amount of health professionals in Australia that are aware of the condition (CIRS Health Professionals, 2018). Most CIRS sufferers who present with a constellation of symptoms typical to CIRS to most GPs or medical specialists will be diagnosed with allergy, ME/CFS, Fibromyalgia or various psychiatric conditions such as depression, anxiety, stress, or PTSD (Common Mold Sickness Misdiagnoses, n.d.).
- Recommendation: Education programs for current GPs and specialists. CIRS diagnosis and treatment information be included in the medical curriculum at universities.
- No NATA/RCPC accredited pathology lab for the majority of biomarkers. The only way to get accurate pathology results at present is by sending bloods on dry ice to Quest diagnostics in the United States. This service is limited to only a small number of practitioners and patients as the cost is approximately $1000, which is prohibitive for many.
- Recommendation: Fast-tracking of accurate test kits for a-MSH, C4a, TGF-b1, VEGF and MMP-9 to an accredited Australian pathology laboratory and these tests be listed on the Medicare schedule.
- Due to the severity of CIRS symptoms, many CIRS patients are bed or house bound, or their geographical distance from their CIRS physician. Thus, a substantial amount of CIRS patients are not able t attend a doctor in person and rely on telephone or videoconferencing. No Medicare rebates are currently available for remote consultations for GPs which raises the cost of medical care substantially.
- Recommendation: CIRS aware specialist GPs, and their patients, be allowed to use MBS video consultation item numbers.
- CIRS is not recognised by any Government department, including The Australian Government Department of Human Services, Medicare and Centrelink, at present. Many doctors will not bulk bill the tests that are currently available for CIRS for fear of AHPRA or Medicare audits.
- Recommendation: Chronic Inflammatory Response Syndrome (CIRS) be included as a valid medical diagnosis for Medicare schedule items and for disability support pension and sickness allowance applications via the Australian Government Department of Human Services/Centrelink.
4. Any intersection with other chronic diseases:
In addition to CIRS-WDB there are several other known CIRS variants, depending on the source of the biotoxin exposure and the patient’s genetic susceptibility (Shoemaker et al., 2018).
- CIRS-Post Lyme Syndrome (CIRS-PLS):Chronic Inflammatory Response Syndrome – Post Lyme Syndrome.
- The bacteria Borrelia burdorgferi and the protozoan Babesia microti also produce biotoxins that can cause CIRS, even if appropriate antibiotic or anti-protozoan agents are given (Shoemaker, Hudnell, House, Van Kempen, & Pakes, 2006; Shoemaker, Giclas, Crowder, House, & Glovsky, 2008).
- CIRS-Ciguatera:
- Ingestion of reef fish with the biotoxin ciguatoxin in susceptible individuals can lead to chronic Ciguatera a.k.a. CIRS-Ciguatera (Shoemaker, House, & Ryan, 2010; Shoemaker, Wu, & Ryan, 2015). Reef fish known to be sources of Ciguatera in Australia, include moray eels, Chinamanfish, Paddletail, Red bass, Spanish Mackerel, Grouper and barracudas among others (Queensland Museum, n.d.; Farrell, Murray, Zammit, & Edwards, 2017).
- CIRS- Dinoflagellates, CIRS-Cyanobacteria:
- A.k.a. Pfiesteria, Possible Estuarine-Associated Syndrome (PEAS), red tide, toxic blue-green algae. An imbalance in the eco-system in water ways can lead to overgrowth of toxin-forming dinoflagellates or cynobacteria, exposure to which (via ingestion of water, inhalation near the water way, or eating marine creatures who reside in the waters) can lead to CIRS (Hudnell, 2005). Pfiesteria was the initial biotoxin that Dr. Shoemaker found among his patients in the mid-1990s (Grattan et al., 1998). Cyanobacterial blooms have been reported in multiple water bodies in Australia and found to produce the toxin β-methylamino-l-alanine which has been linked to neurodegenerative diseases such as Alzheimer’s disease, amyotrophic lateral sclerosis (ALS) and Parkinson’s disease (Main, 2018; Main et al., 2018).
- CIRS-WDB/SBS/DMHS or fungal and/or mycotoxin exposure have also been associated with:
- Chronic Fatigue Syndrome: The symptoms of ME/CFS and CIRS overlap almost 100% (Bijlsma, 2017). Both conditions are multi-symptom, multisystem disorders that can profoundly affect quality of life, causing extreme fatigue, gastrointestinal disturbances, impaired cognition, neurological symptoms, flu-like symptoms, chemical sensitivity, PENE (Chester & Levine, 1994, 1997; Shoemaker & Maziel, 2009; Brewer, Thrasher, & Hooper, 2013; Morris, Berk, Walder, & Maes, 2016; Gunn, Gunn, & Mueller, 2016). One of the original mid-1980s Tahoe-Truckee CFS cluster patients, Erik Johnson, is a member and frequent contributor to the TMSA Facebook group. By fastidiously avoiding mould he regained his health and as long as he continues to avoid it, he remains largely symptom free (Petrison, 2013).
- Alzheimer’s disease: Dr. Dale Bredesen has theorised one of the three subtypes of Alzheimer’s disease, Toxic/inhalational Alzheimer’s, is a phenotype of CIRS (Bredesen, 2016; Bredesen et al., 2016).
- Multiple Chemical Sensitivity (MCS): Many of those with CIRS also have concurrent MCS (Tuuminen, Sakari Rinee, 2017; Valtonen, 2017; Rea, 2016).
- Lower IQ and developmental delays in children (Jedrychowski et al., 2011).
- Depression (Shenassa et al., 2007; Amritwar et al., 2017).
- Mast cell disorders (Ratnaseelan, Tsilioni, & Theoharides, 2018; Theoharides, Stewart, Hatziagelaki & Gerasimos Kolaitis, 2015).
- Sarcoidosis (Tercelj, Salobir, Harlander, & Rylander, 2011; Rossman et al., 2008; Newman et al., 2004).
- Autism Spectrum Disorders (Ratnaseelan et al., 2018).
- Ulcerative colitis (Gunn et al., 2016).
5. Investment in contemporary Australian research to discover and provide evidence of CIRS as a chronic, multisystem disease: & 6. Research into biotoxin-related illness caused from water damaged buildings:
There is an urgent need for epidemiological studies to determine the prevalence of CIRS-WDB and genetic susceptibility in the Australian population.
In addition the prevalence of water-damaged buildings, both private, commercial and public needs to be determined. Australian clinical studies, based on previous peer reviewed research (Shoemaker et al., 2006; Shoemaker et al., 2013) should also be funded.
Recommendation: Funding provided for epidemiological and clinical studies to determine the prevalence and incidence of CIRS-WDB and water-damaged buildings. Also studies are needed to determine the most efficacious clinical treatments for patients. These may involve organisations, such as ACIIDS, Australasian College of Nutritional and Environmental Medicine, Australian Integrative Medicine Association and the Australian Society of Building Biologists (ASBB, n.d.).
7. Any related matters:
Any discussion on CIRS-WDB must include a focus on the built environment and water-damaged buildings. Simply put, if buildings were designed, constructed and maintained so they never became water-damaged there would be no CIRS-WDB.
There are three main causes of water damage to buildings:
- Design/construction flaws and lack of maintenance: This is the leading cause of water damage and is due to building design flaws, faulty construction methods, water damage during construction, and lack of building maintenance (including air conditioner maintenance) or appliance leaks.
- Natural events: Floods, cyclones, storms and hail. Many populous areas of Australia are at risk of flooding or storm damage that can cause serious water ingress (Katelaris, 2013).
- Occupant behaviour: Internal flooding of sinks or baths, constantly keeping windows shut, too many people for the space. While this is a factor it is one overemphasised by the insurance and real estate industries, when the underlying fault is due to the design, construction or maintenance flaws.
Note: Amplified fungal and bacterial growth can occur after 48 hours of moisture saturation or ingress.
Issues facing Australian housing and buildings as related to indoor air quality and water damage:
- Design and construction of water-tight and breathable buildings:
- The Australian building code has been focused on making buildings increasingly energy efficient and fireproof at the expense of limiting condensation and allowing water vapour to escape (Dewsbury, & Law, 2017). The Australian Building Codes Board (ABCB) has published a non-mandatory guide for condensation in buildings (2014) and funded a scoping study (Dewsbury et al., 2016) which provide education and design and building guidelines to prevent this.
- The World Health Organization (2009) states:“Well-designed, well-constructed, well-maintained building envelopes are critical to the prevention and control of excess moisture and microbial growth, as they prevent thermal bridges and the entry of liquid or vapour-phase water. Management of moisture requires proper control of temperatures and ventilation to avoid excess humidity, condensation on surfaces and excess moisture in materials. Ventilation should be distributed effectively throughout spaces, and stagnant air zones should be avoided.”
- Recommendation: For the ABCB building code to incorporate the ABCB Condensation in buildings handbook and scoping study guidelines. A remediation program be instigated for buildings already built to the current building code to mitigate condensation issues.
- Testing of water-damaged buildings:
- Testing of buildings for water damage is currently done by indoor environmental professionals (IEP), certified occupational hygienists (COH), mycologists, building biologists, remediators and occupants themselves using kits mailed back to mycologists. Methods of testing include visual inspection, moisture readings, infrared readings, particle counts, VOC and gas measurements, spore trap air sampling, tape lifts/surface sampling and MSQPCR dust sampling. Testing buildings for patients with CIRS-WDB should include QPCR and the HERTSMI-2 score as part of the testing (Shoemaker, & Lark, 2016).
- Recommendation: Disallowing remediators to test themselves as this is an obvious conflict of interest.
- Remediation of water-damaged buildings:
- The Australian mould remediation industry is currently one without regulation, recourse or accountability. A major trend in this country is to remediate water damage and fungal growth by using gassing, fogging or spraying of biocides to kill microbes in place of source removal. This practice is dangerous for those with CIRS-WDB as fungi and their fragments are even more toxic when dead than when living.
- Substituting fogging for mould removal goes against the international ANSI/IICRC standard (ANSI/IICRC ii, 2015) states: “5.8.1 Chemicals (Antimicrobials and Biocides) Source removal of mold contamination should always be the primary means of remediation. Indiscriminate use of antimicrobials, coatings, sealants, and cleaning chemicals is not recommended.” Remediation for CIRS-WDB patients will often need to be even of even a higher level than the ANSI/IICRC standard. This level is outlined in the Surviving Mold consensus statement (Schwartz et al., 2016). Assessors, insurance companies and landlords will often award jobs to mould remediators based on cost or speed rather than following ANSI/IICRC standards.
- Recommendation: An accreditation or regulation program for mould remediators be implemented so the consumer is aware that they follow ANSI/IICRC standards. Remediators who are chosen by assessors, insurance companies, real estate agencies or landlords must follow ANSI/IICRC standards at a minimum.
- Tenancy legislation:
- There is no mention of mould in any of the state tenancy laws in Australia, instead relying on nonspecific clauses such as “protection from damp and its effects” and “ventilation and insulation” (Residential Tenancies and Rooming Accommodation Act, p32)
- Recommendation: Amendments to Australia’s tenancy laws, similar to California’s (United States) Senate Bill 655 which adds visible mold growth to the list of dangerous health conditions which define substandard housing in that state’s Health and Safety Code (SB-655 Housing standards: mold, n.d.).
- Testing and remediation of public buildings:
- Public housing and social housing that provide living accommodation for people with low incomes, Aboriginal Australians and refugees and asylum seekers have high rates of water damage and dampness (McPherson, 2018, August 1; Anderson, Williamson, Fernando, Wright, & Redman, 2018; Ziersch, Walsh, Clemence, & Duivesteyn, 2017; Baker et al, 2017).
- The World Health Organization (2009) states: “Dampness and mould may be particularly prevalent in poorly maintained housing for low-income people. Remediation of the conditions that lead to adverse exposure should be given priority to prevent an additional contribution to poor health in populations who are already living with an increased burden of disease.”
- People on low incomes are also the ones least able to afford CIRS medical treatment and housing remediation or relocation. Hospitals, libraries, emergency services offices, prisons, armed forces accommodation, primary and secondary schools and universities are frequently reported in TMSA, the media (McPherson, 2018, May 14) and the literature as having significant water damage also.
- Recommendation: While changing the building code will help future buildings, a testing and remediation program for current public buildings is desperately needed.
Conclusion
CIRS-WDB is an emerging public health issue facing the Australian population. It causes a great deal of suffering, disability and financial cost to those who suffer from it. It also impacts the government financially, both directly by increased health care and social security costs and indirectly via loss of CIRS-WDB patients in the workforce. By acting swiftly the Australian government can help those currently suffering from this condition and prevent future cases of CIRS-WDB by funding research, public health awareness programs, modification of building codes and initiating remediation and accreditation programs.
References
Anderson, M.J., Williamson, A.B., Fernando, P., Wright, D., & Redman, S. (2018). Housing conditions of urban households with Aboriginal children in NSW Australia: tenure type matters. BMC Public Health, 18(70). doi: 10.1186/s12889-017-4607-y PMC5540447
ANSI/IICRC i. (2015). ANSI/IICRC R520 Reference guide for professional mold remediation – third edition. Institute of inspection cleaning and restoration certification. https://www.iicrc.org
ANSI/IICRC ii. (2015). ANSI/IICRC S520 Standard for professional mold remediation – third edition. Institute of inspection cleaning and restoration certification. https://www.iicrc.org
Australian Bureau of Statistics. (2018). 31.01.0 – Australian Demographic Statistics, Dec 2017. Retrieved from http://www.abs.gov.au/ausstats/abs@.nsf/0/D56C4A3E41586764CA2581A70015893E?Opendocument
Australian Building Codes Board (ABCB). (2014). Condensation in buildings handbook second edition. Retrieved from http://www.abcb.gov.au/Resources/Publications/Education-Training/Condensation-in-Buildings
Australian Chronic Infectious & Inflammatory Disease Society (ACIIDS). (n.d.). Retrieved from https://www.aciids.org.au/
Australian Society of Building Biologists (ASBB). (n.d.). Retrieved from http://asbb.org.au/
Baker, E., Beer, A., Lester, L., Pevalin, D. Whitehead, C. & Bently, R. (2017). Is housing a health insult? Int J Environ Res Public Health, 14(6): 567. Doi: 10.3390/ijerph14060567 PMC5486253
Berndtson, K., McMahon, S., Ackerley, M., Rapaport, S., Gupta, S., & Shoemaker, R. (2016). Medically sound investigation and remediation of water-damaged buildings in cases of chronic inflammatory response syndrome. Center for research on biotoxin associated illness, Pocokomoke, MD. Retrieved from https://www.survivingmold.com/docs/MEDICAL_CONSENSUS_1_19_2016_INDOOR_AIR_KB_FINAL.pdf
Berry, Y. (2014). The physicians guide to understanding and treating biotoxin illness. Surviving Mold. Retrieved from https://www.survivingmold.com/legal-resources/works-citing-dr.-shoemaker/a-physicians-guide-to-biotoxin-illness
Bijlsma, N. (2017). Healthy home healthy family: Is where you live affecting your health? Australian college of environmental studies.
Bodis, G., Toth, V., & Schwarting, A. (2018). Role of Human Leukocyte Antigens (HLA) in Autoimmune Diseases. Rheumatol therapies, 5(1):5-20. doi: 10.1007/s40744-018-0100-z PMC5935613
Bredesen, D.E., Amos, E.C.,Canick, J., Ackerley, M., Raji, C., Milan, F., M.F, & Ahdidan, J. (2016). Reversal of cognitive decline in Alzheimer’s disease. Aging, 8(6), 1250-1258. doi: 10.18632/aging.100981 PMC4931830 PMID 27294343
Bredesen D.E. (2016). Inhalational Alzheimer’s disease: an unrecognized – and treatable – epidemic. Aging, 8(2), 304-13. PMC4789584 PMID 26870879
Brewer, J., Thrasher, J., Straus, D., Madison, R. & Hooper, D. (2013). Detection of mycotoxins in patients with chronic fatigue syndrome. Toxins, 5(4), 605-17. doi: 10.3390/toxins5040605 PMC2705282 PMID 23580077
Campbell, A.W., Thrasher, J.D., Gray, M.R. & Vojandi, A. (2004). Mold and Mycotoxins: Effects on the Neurological and Immune Systems in Humans. Advances in applied microbiology, 55, 375-406. PMID 15350803
Chester, A.C., & Levine, P.H. (1994). Concurrent sick building syndrome and chronic fatigue syndrome: epidemic neuromyasthenia revisited. Clinical infectious diseases, 18 Suppl 1,S43-8. PMID 8148452
Chester, A.C., & Levine, P.H. (1997). The natural history of concurrent sick building syndrome and chronic fatigue syndrome. Journal of psychiatric research, 31(1),51-7. PMID 9201647
CIRS Health Professionals. (2018). Retrieved from https://www.toxicmould.org/health-professionals/
Daschner, A. (2016). An Evolutionary-Based Framework for Analyzing Mold and Dampness-Associated Symptoms in DMHS. Frontiers in Immunology, 7: 672. doi: 10.3389/fimmu.2016.00672 PMC5220099
Dewsbury, M., Law, T., Potgieter, J., Fitz-Gerald, D., McComish, B., Chandler, T. & Soudan, A. (2016). Scoping study of condensation in residential buildings. Australian building codes board. Retrieved from http://www.abcb.gov.au/Resources/Publications/Research/Scoping-Study-of-Condensation-in-Residential-Buildings
Dewsbury, M., Law, T. (2017). Temperate climates, warmer houses and built fabric challenges. Procedia engineering, 180, 1065-1074 doi: 10.1016/j.proeng.2017.04.266
FAQ. (n.d.). Retrieved from https://www.toxicmould.org/faq/
Farrell, H., Marruay, S.A., Zammit, A., & Edwards, A.W. (2017). Management of ciguatoxin risk in Eastern Australia. Toxins (Basel), 9(11): 367. doi: 10.3390/toxins9110367 PMC5705982
Global indoor health network (GIHN). (2018). Diagnosis and treatment of illness caused by contaminants in water-damaged buildings. Retrieved from https://www.globalindoorhealthnetwork.com/GIHN-papers
Grattan, L.M., Oldach, D., Perl, T.M., Lowitt, Matuszak, D.L., Dickson, C., Parrott, C., Shoemaker, R.C., Kauffman, C.L., Wasserman, M.P., Hebel, J.R., Charache, P., & Morris, J.G. (1998). Learning and memory difficulties after environmental exposure to waterways containing toxin-producing Pfiesteria or Pfiesteria-like dinoflagellates. Lancet, 352 (1998), 532–539. doi: 10.1016/S0140-6736(98)02132-1 PMID 9716058
Gray, M., Thrasher, J., Crago, R., Madison, R., Arnold, L., Campbell, W., & Vojdani, A. (2003). Mixed mold mycotoxicosis: immunological changes in humans following exposure in water-damaged buildings. Archives of environmental health, 58(7), 410-420. PMID 15143854
Gunn, S.R., Gunn, G.G., & Mueller, F.W. (2016). Reversal of refractory ulcerative colitis and severe chronic fatigue syndrome symptoms arising from immune disturbance in an HLA-DR/DQ genetically susceptible individual with multiple biotoxin exposures. American journal of case reports, 2016(17), 320–325. doi: 10.12659/AJCR.896949 PMC4913732
HLA-DR Haplotype Definitions – 4-3-53. (n.d.). Retrieved from http://www.myhousemakesmesick.com/hlacalc/4-3-53.php
HLA Panel Screen (DR and DQ). (2015, May 31). Sonic genetics. Retrieved from https://www.sonicgenetics.com.au/tests/hla-panel-screen-dr-and-dq/
Hooper, D., Bolton, V., Guilford, F., & Straus, D. (2009). Mycotoxin detection in human samples from patients exposed to environmental molds. International journal of molecular sciences, 10(4), 1465–75. doi: 10.3390/ijms10041465 PMC2680628 PMID 19468319
Hope, J. (2013). A review of the mechanism of injury and treatment approaches for illness resulting from exposure to water damaged buildings, mold, and mycotoxins. The scientific world journal, Apr 18,767482. doi: 10.1155/2013/767482 PMC2654247 PMID 23710148
Hudnell, H.K. (2005). Chronic biotoxin-associated illness: multiple-system symptoms, a vision deficit, and effective treatment. Neurotoxicology and teratology, 27(5), 733-43. PMID 16102938
International Society for Environmentally Acquired Illness (ISEAI). (n.d.). Retrieved from https://iseai.org/
Jedrychowski, W., Maugeri, U., Perera, F., Stigter, L., Jankowski, J., Butscher, M., Mroz, E., Flak, E., Skarupa, A., & Sow, A. (2011). Cognitive function of 6-year old children exposed to mold-contaminated homes in early postnatal period. Prospective birth cohort study in Poland. Physiology & behaviour, 104(5):989-95. doi: 10.1016/j.physbeh.2011.06.019 PMID 21763705
Katelaris, C. (2013, December 6). Queenslanders at risk from mould as flood clean-up continues. TheConversation.com. Retrieved from https://theconversation.com/queenslanders-at-risk-from-mould-as-flood-clean-up-continues-11935
Lab tests for mold illness. (n.d.). Surviving Mold. Retrieved from https://www.survivingmold.com/diagnosis/lab-tests
Main, B.J, Bowling, L.C., Padulaa, M.P., Bishop, D.P., Mitrovic, S.M., Guillemin, G.J., & Rodgers, K.J. (2018). Detection of the suspected neurotoxin β-methylamino-l-alanine (BMAA) in cyanobacterial blooms from multiple water bodies in Eastern Australia. Harmful algae, 74, April 2018, 10-18. doi: 10.1016/j.hal.2018.03.004 PMID 29724339
Main, B. (2018, May 7). Toxin linked to motor neuron disease found in Australian algal blooms. The Conversation. Retrieved from https://theconversation.com/toxin-linked-to-motor-neuron-disease-found-in-australian-algal-blooms-95646
McMahon, S. (2017). An Evaluation of Alternate Means to Diagnose Chronic Inflammatory Response Syndrome and Determine Prevalence. Medical research archives, 5(3), March 2017. doi: 10.18103/mra.v5i3.1125 Retrieved from https://www.survivingmold.com/Publications/ALTERNATE_MEANS_-_FINAL_GALLEY_-_3-2017.PDF
McMahon, S., Kundomal, K., & Yangalasetty, S. (2017). Pediatrics Norms for Visual Contrast Sensitivity Using an APT VCS Tester. Medical research archives, 5(5) May 2017.
doi: 10.18103/mra.v5i5.1295 Retrieved from https://www.survivingmold.com/Publications/PEDS_VCS_-_FINAL_GALLEY_-_5-8-2017.PDF
McPherson. (2018, May 14). Girl fell ‘dangerously ill’ after mould exposure at NSW School, mum says. 9news.com.au. Retrieved from https://www.9news.com.au/national/2018/05/14/13/07/girl-falls-dangerously-ill-after-mould-exposure-at-nsw-school-mum-says
McPherson. (2018, August 1). Canberra mum ‘hospitalised 160 times’ due to mould-infested public housing home. 9news.com.au. Retrieved from https://www.9news.com.au/national/2018/08/01/12/53/canberra-mum-hospitalised-160-times-due-to-mould-infested-public-housing-home
Media, Building Code and Government Links. (2018). Retrieved from https://www.toxicmould.org/media-links/
Mould: Everything you didn’t want to know. (n.d.). Tenantsrights.org.au. Retrieved from http://www.tenantsrights.org.au/Publications_Archive/MOULD%20-%20Everything%20you%20didnt%20want%20to%20know.pdf
Morris, G., Berk, M., Walder, K., & Maes, M. (2015). The putative role of viruses, bacteria, and chronic fungal biotoxin exposure in the genesis of intractable fatigue accompanied by cognitive and physical disability. Molecular neurobiology, 53(4), 2550-71. doi: 10.1007/s12035-015-9262-7 PMID 26081141
Nakayama, K. & Morimoto, K. (2007). Relationship between, lifestyle, mold and sick building syndromes in newly built dwellings in Japan. Int J Immunopathol Pharmacol, 20(2 Suppl 2),35-43. PMID 17903355
Newman, L.S., Rose, C.S., Bresnitz, E.A., Rossman, M.D., Barnard, J., Frederick, M., Terrin, M.L., Weinberger, S.E., Moller, D.R., McLennan, G., Hunninghake, G., DePalo, L., Baughman, R.P., Iannuzzi, M.C., Judson, M.A., Knatterud, G.L., Thompson, B.W., Teirstein, A.S., Yeager, H. Jr., Johns, C.J., Rabin, D.L., Rybicki, B.A., Cherniack, R., & Group, A.R. (2004). A case control etiologic study of sarcoidosis: environmental and occupational risk factors. American journal of respiratory and critical care medicine, 170(12):1324-30. doi: 10.1164/rccm.200402-249OC PMID 15347561
Online VCS Screening Test. (n.d.). Surviving Mold. Retrieved from https://www.survivingmold.com/store1/online-screening-test
Petrison, L. (2013). Back from the Edge: How One Man’s Discovery Brought Him from Desperately Sick with Chronic Fatigue Syndrome to the Top of Mt. Whitney in Six Months Paradigm change. Retrieved from http://paradigmchange.me/
Queensland museum. (n.d.). Ciguatoxic fishes. Retrieved from http://www.qm.qld.gov.au/Find+out+about/Animals+of+Queensland/Fishes/Fish+poisoning/Ciguatoxic+fishes#.W16NstIzaiM
Ratnaseelan, A.M., Tsilioni, I., & Theoharides, T.C. (2018). Effects of mycotoxins on neuropsychiatric symptoms and immune processes. Clinical therapies, 40(6):903-917. doi: 10.1016/j.clinthera.2018.05.004. PMID 29880330
Rea, W.J. (2016). History of chemical sensitivity and diagnosis. Reviews on environmental health, 31(3):353-61. doi: 10.1515/reveh-2015-0021 PMID 27383867
Residential Tenancies and Rooming Accommodation Act 2008. (2018). State of Queensland. Retrieved from https://www.legislation.qld.gov.au/view/pdf/inforce/current/act-2008-073
Rossman, M.D, Thompson, B., Frederick, M., Iannuzzi, M.C., Rybicki, B.A., Pander, J.P., Newman, L.S., Rose, C., Magira, E., & Monos, D. (2008). HLA and environmental interactions in sarcoidosis. Sarcoidosis, vasculitis, and diffuse lung diseases, 25(2):125-32. PMID 19382531
SB-655 Housing standards: mold. (n.d.) California legislative information. Retrieved from https://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=201520160SB655
Shenassa, E.D., Daskalakis, C., Liebhaber, A., Braubach, M. & Brown M. (2007). Dampness and mold in the home and depression: an examination of mold-related illness and perceived control of one’s home as possible depression pathways. American journal of public health, 97(10):1893-9. PMC1994167 PMID 17761567
Schwartz, L., Weatherman, G., Schrantz, M., Spates, W., Charlton, J., Berndtson, K., & Shoemaker. R. (2016). Indoor environmental professionals panel of surviving mold – consensus statement. Survivingmold.com. Retrieved from https://www.survivingmold.com/docs/IEP_CONSENSUS_04_12_16.pdf
Shoemaker, R. (2010). Surviving Mold – life in the era of dangerous buildings. Otter bay books.
Shoemaker, R.C., Giclas, P, Crowder, C, House, D.E., & Glovsky, M. (2008). Complement split products C3a and C4a are early markers of acute Lyme disease in tick bite patients in the United States. International archives of allergy and immunology, 146(3), 255-61. doi: 10.1159/000116362 PMID 18270493
Shoemaker, R.C., & House, D.E. (2006). Sick building syndrome (SBS) and exposure to water-damaged buildings: time series study, clinical trial and mechanisms. Neurotoxicology and teratology, 28(5), 573-88. PMID 17010568 Retrieved from https://www.survivingmold.com/docs/Resources/Shoemaker%20Papers/NTT5863.pdf
Shoemaker, R.C., House, D.E., & Ryan, J.C. (2013). Vasoactive intestinal polypeptide (VIP) corrects chronic inflammatory response syndrome (CIRS) acquired following exposure to water-damaged buildings. Health, 5(3) 2013, 396-401. doi: 10.4236/health.2013.53053 Retrieved from http://www.scirp.org/journal/PaperInformation.aspx?PaperID=28586
Shoemaker, R.C., House, D.E., & Ryan, J.C. (2014). Structural brain abnormalities in patients with inflammatory illness acquired following exposure to water-damaged buildings: A volumetric MRI study using NeuroQuant. Neurotoxicology and teratology, 45, 18-26. doi: 10.1016/j.ntt.2014.06.004 PMID 24946038 Retrieved from https://www.survivingmold.com/docs/NTT_NQ_PDF_06_17_2014.PDF
Shoemaker, R.C., Johnson, K., Lysander, J., Berry, Y., Dooley, M., Ryan, J. & McMahon, S. (2018). Diagnostic process for chronic inflammatory response syndrome (CIRS): A consensus statement report of the consensus committee of surviving mold. Internal medicine review, 4(5) May 2018. Retrieved from https://www.survivingmold.com/Publications/CIRS_diagnostic_protocol_final_5_1_2018.pdf
Shoemaker, R.C., & Lark, D. (2016). HERTSMI-2 and ERMI: Correlating Human Health Risk with Mold Specific qPCR in Water-Damaged Buildings. Proceedings of the 14th International Conference on Indoor Air Quality and Climate, International Society for Indoor Air Quality and Climate, Ghent, Belgium. Retrieved from https://www.isiaq.org/docs/Papers/Paper658.pdf
Shoemaker, R.C., Hudnell, H.K., House, D.E., Van Kempen, A., & Pakes, G. (2006). Atovaquone plus cholestyramine in patients coinfected with Babesia microti and Borrelia burgdorferi refractory to other treatment. Advances in therapy, 23(1), 1-11. PMID 16644602 Retrieved from https://www.survivingmold.com/docs/Resources/Shoemaker%20Papers/23_1_1-111.pdf
Shoemaker, R.C. & Maziel, M.S. (2009). Exposure to interior environments of water-damaged buildings causes a CFS-like illness in pediatric patients: a case/control study. Bulletin of the IACFS/ME 2009, 17(2). Retrieved from http://www.iacfsme.org/Portals/0/pdf/Shoemaker%20vol17%20n2.pdf
Straus, D.C. (2011). The possible role of fungal contamination in sick building syndrome. Front Biosciences (Elite Ed), 1(3),562-80. PMID 21196335
Steere, A.C., Klitz, W., Drouin, E.E., Falk, B.A., Kwok, W.W., Nepom, G.T. & Baxter-Lowe, L.A. (2006). Antibiotic-refractory Lyme arthritis is associated with HLA-DR molecules that bind a Borrelia burgdorferi peptide. The journal of experimental medicine, 203(4),961-71, PMID 16585267
Takaoka, M., Suzuki, K. & Norbäck, D. (2016). Sick Building Syndrome among Junior High School Students in Japan in Relation to the Home and School Environment. Glob J Health Sci. 2015 Jun 12;8(2):165-77. doi: 10.5539/gjhs.v8n2p16 PMC4803974
Terčelj, M., Salobir,B., Harlander, M., & Rylander, R. (2011). Fungal exposure in homes of patients with sarcoidosis – an environmental exposure study. Environ Health, 10: 8. doi: 10.1186/1476-069X-10-8 PMC3036600
Toxic Mould Support Australia Facebook Group. (n.d.). Retrieved from https://www.facebook.com/groups/toxicmouldsupportaustralia
Toxic Mould Support Australia. (n.d.). Retrieved from https://www.toxicmould.org
Thrasher, J.D. (2016). Fungi, bacteria, nano-particulates, mycotoxins and human health in water-damaged indoor environments. Journal of community and public health nursing, 2(2). doi: dx.doi.org/10.4172/jcphn.1000115
Tuuminen, T & Sakari Rinne, K. (2017). Severe Sequelae to Mold-Related Illness as Demonstrated in Two Finnish Cohorts. Frontiers of immunology, 8, 382. doi: 10.3389/fimmu.2017.00382 PMC5377931
U.S. Government Accountability Office (U.S. GAO). (2008). Indoor mold: better coordination of research on health effects and more consistent guidance would improve federal efforts. GAO-08-980. Retrieved from https://www.gao.gov/products/GAO-08-980
Valtonen V. (2017). Clinical diagnosis of the dampness and mold hypersensitivity syndrome: review of the literature and suggested diagnostic criteria. Frontiers in Immunology, 10(8),951. doi: 10.3389/fimmu.2017.00951 PMID 28848553
World Health Organization Europe. (2009). WHO guidelines for indoor air quality: dampness and mould. World Health Organization, Geneva. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK143941/
Ziersch, A., Walsh, M., Due, Clemence, Duivesteyn, E. (2017). Exploring the Relationship between Housing and Health for Refugees and Asylum Seekers in South Australia: A Qualitative Study. Int J Environ Res Public Health, 14(9), 1036. PMC5615573



Leave A Comment
You must be logged in to post a comment.