A subset of the Biotoxin Research Database, this graphical timeline represents the key papers regarding chronic multisystem illness due to damp/water-damaged buildings, and related biotoxin illnesses, from the mid 1980s to present.
SEARCH TERMS & ACRONYMS
- Biotoxin illness
- BRI = Building Related Illnesses
- CFS = Chronic Fatigue Syndrome
- CIRS = Chronic Inflammatory Response Syndrome
- DBRI = Damp Building-Related Illnesses
- DMHS = Dampness and Mold Hypersensitivity Syndrome
- MCS = Multiple Chemical Sensitivity
- SBS = Sick Building Syndrome
- VIP = Vasoactive Intestinal Polypeptide
- WDB = Water-damaged Building
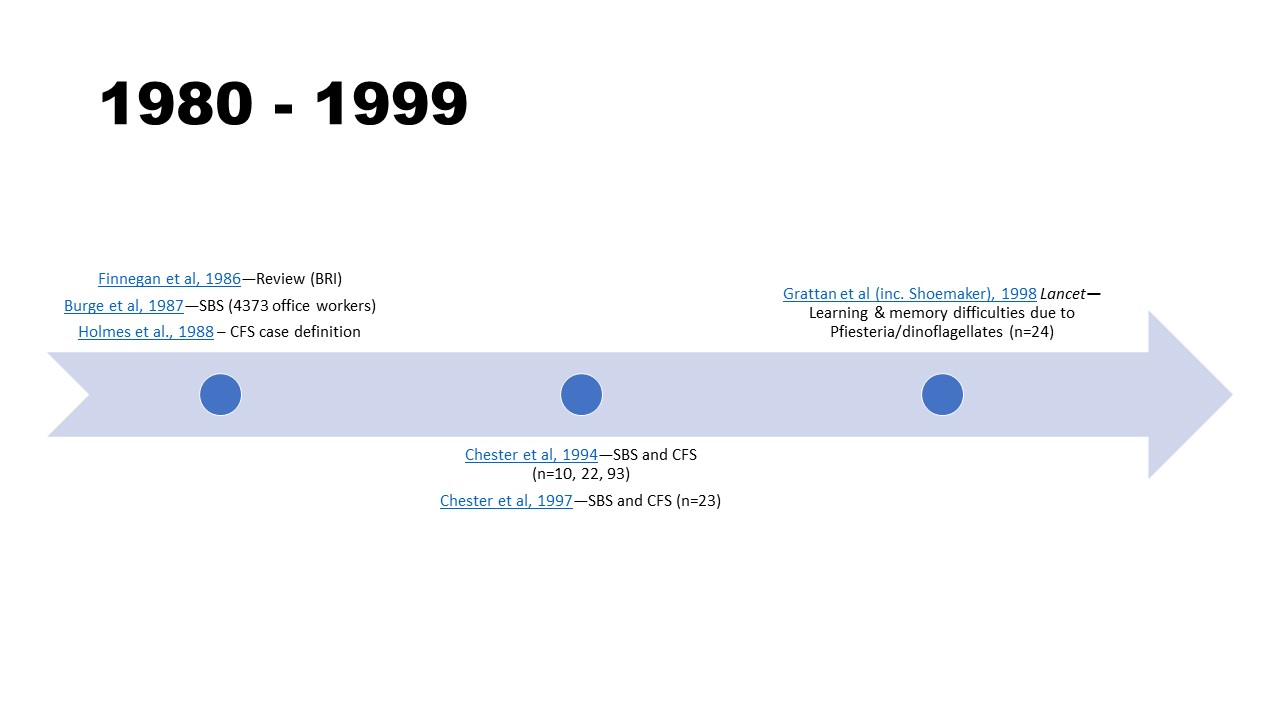
1980 – 1999
- Finnegan, M. J., & Pickering, C. A. (1986). Building related illness. Clinical allergy, 16(5), 389–405. https://doi.org/10.1111/j.1365-2222.1986.tb01974.x
- Burge, S., Hedge, A., Wilson, S., Bass, J. H., & Robertson, A. (1987). Sick building syndrome: a study of 4373 office workers. The Annals of occupational hygiene, 31(4A), 493–504. https://doi.org/10.1093/annhyg/31.4a.493
- Holmes, G. P., Kaplan, J. E., Gantz, N. M., Komaroff, A. L., Schonberger, L. B., Straus, S. E., Jones, J. F., Dubois, R. E., Cunningham-Rundles, C., & Pahwa, S. (1988). Chronic fatigue syndrome: a working case definition. Annals of internal medicine, 108(3), 387–389. https://doi.org/10.7326/0003-4819-108-3-387
- Chester, A. C., & Levine, P. H. (1994). Concurrent sick building syndrome and chronic fatigue syndrome: epidemic neuromyasthenia revisited. Clinical infectious diseases, 18 Suppl 1, S43–S48. https://doi.org/10.1093/clinids/18.supplement_1.s43
- Chester, A. C., & Levine, P. H. (1997). The natural history of concurrent sick building syndrome and chronic fatigue syndrome. Journal of psychiatric research, 31(1), 51–57. https://doi.org/10.1016/s0022-3956(96)00054-4
- Grattan, L.M., Oldach, D., Perl, T.M., Lowitt, M.H., Matuszak, D.L., Dickson, C., Parrott, C., Shoemaker, R.C., Kauffman, C.L, Wasserman, M.P., Hebel, J.R., Charache, P. & Morris Jr, J.G. (1998). Learning and memory difficulties after environmental exposure to waterways containing toxin-producing Pfiesteria or Pfiesteria-like dinoflagellates. Lancet, 353(9127):532-9. https://doi.org/10.1016/s0140-6736(98)02132-1
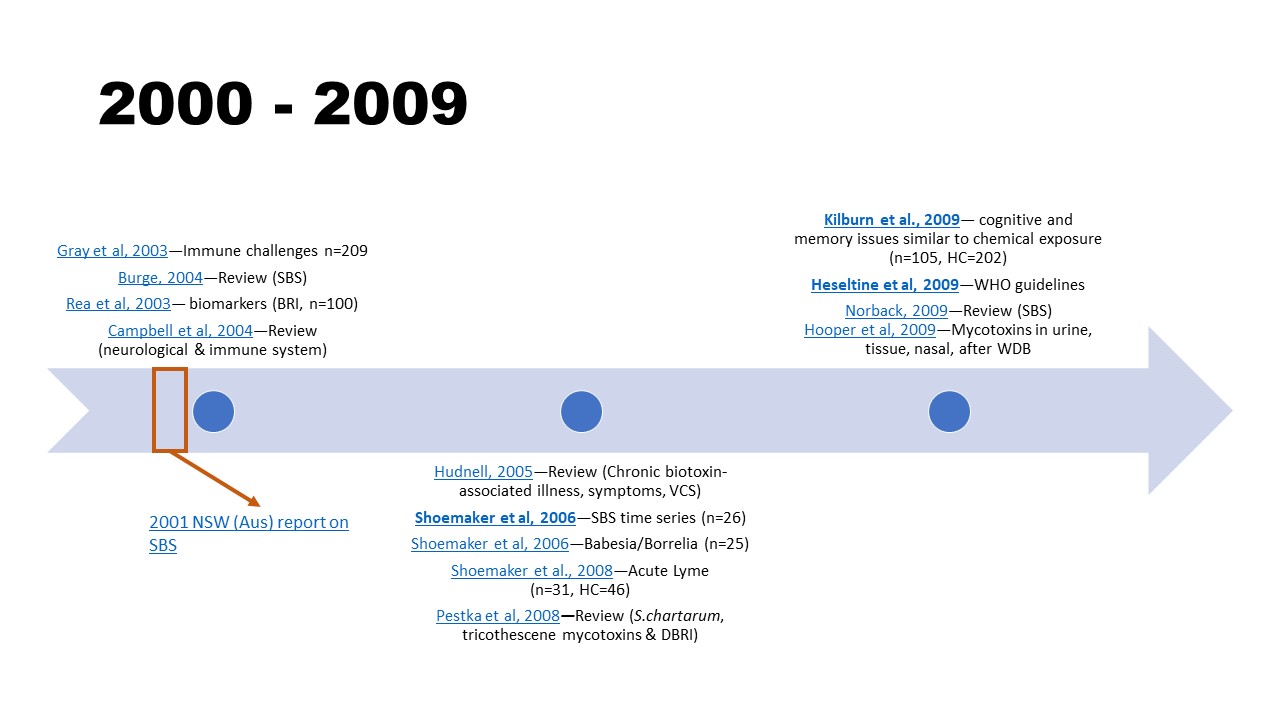
2000 – 2009
- Gray, M. R., Thrasher, J. D., Crago, R., Madison, R. A., Arnold, L., Campbell, A. W., & Vojdani, A. (2003). Mixed mold mycotoxicosis: immunological changes in humans following exposure in water-damaged buildings. Archives of environmental health, 58(7), 410–420. https://doi.org/10.1080/00039896.2003.11879142
- Burge P. S. (2004). Sick building syndrome. Occupational and environmental medicine, 61(2), 185–190. https://doi.org/10.1136/oem.2003.008813
- Campbell, A. W., Thrasher, J. D., Gray, M. R., & Vojdani, A. (2004). Mold and mycotoxins: effects on the neurological and immune systems in humans. Advances in applied microbiology, 55, 375–406. https://doi.org/10.1016/S0065-2164(04)55015-3
- Report of the Standing Committee on Public Works. (2001). Sick Building Syndrome (Report No. 52/07). NSW Parliament (PDF)
- Hudnell, H.K. (2005). Chronic biotoxin-associated illness: multiple-system symptoms, a vision deficit, and effective treatment. Neurotoxicology and teratology, 27(5), 733-43. https://doi.org/10.1016/j.ntt.2005.06.010
- Shoemaker, R. C., & House, D. E. (2006). Sick building syndrome (SBS) and exposure to water-damaged buildings: time series study, clinical trial and mechanisms. Neurotoxicology and teratology, 28(5), 573–588. https://doi.org/10.1016/j.ntt.2006.07.003
- Shoemaker, R. C., Hudnell, H. K., House, D. E., Van Kempen, A., Pakes, G. E., & COL40155 Study Team (2006). Atovaquone plus cholestyramine in patients coinfected with Babesia microti and Borrelia burgdorferi refractory to other treatment. Advances in therapy, 23(1), 1–11. https://doi.org/10.1007/BF02850341
- Shoemaker, R. C., Giclas, P. C., Crowder, C., House, D., & Glovsky, M. M. (2008). Complement split products C3a and C4a are early markers of acute lyme disease in tick bite patients in the United States. International archives of allergy and immunology, 146(3), 255–261. https://doi.org/10.1159/000116362
- Pestka, J. J., Yike, I., Dearborn, D. G., Ward, M. D., & Harkema, J. R. (2008). Stachybotrys chartarum, trichothecene mycotoxins, and damp building-related illness: new insights into a public health enigma. Toxicological sciences, 104(1), 4–26. https://doi.org/10.1093/toxsci/kfm284
- Kilburn, K. H. (2009). Neurobehavioral and pulmonary impairment in 105 adults with indoor exposure to molds compared to 100 exposed to chemicals. Toxicology and Industrial Health, 25(9–10), 681–692. https://doi.org/10.1177/0748233709348390
- Heseltine, E., & Rosen, J. (Eds.). (2009). WHO guidelines for indoor air quality: dampness and mould. World Health Organization, Geneva. NBK143941.
- Norbäck D. (2009). An update on sick building syndrome. Current opinion in allergy and clinical immunology, 9(1), 55–59. https://doi.org/10.1097/ACI.0b013e32831f8f08
- Hooper, D., Bolton, V., Guilford, F., & Straus, D. (2009). Mycotoxin Detection in Human Samples from Patients Exposed to Environmental Molds. International Journal of Molecular Sciences, 10(4), 1465–1475. MDPI AG. http://dx.doi.org/10.3390/ijms10041465
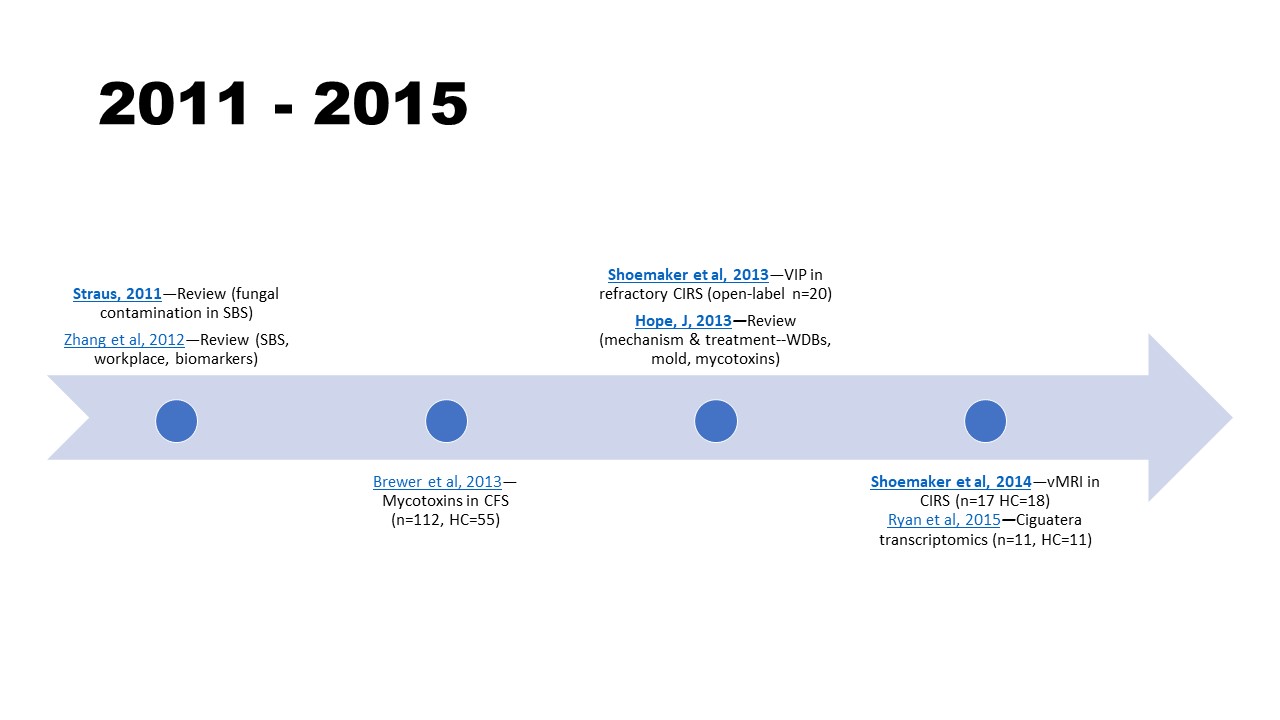
2011 – 2015
- Straus D. C. (2011). The possible role of fungal contamination in sick building syndrome. Frontiers in bioscience (Elite edition), 3, 562–580. https://doi.org/10.2741/e270
- Zhang, X., Sahlberg, B., Wieslander, G., Janson, C., Gislason, T., & Norback, D. (2012). Dampness and moulds in workplace buildings: associations with incidence and remission of sick building syndrome (SBS) and biomarkers of inflammation in a 10 year follow-up study. The Science of the total environment, 430, 75–81. https://doi.org/10.1016/j.scitotenv.2012.04.040
- Brewer, J. H., Thrasher, J. D., Straus, D. C., Madison, R. A., & Hooper, D. (2013). Detection of mycotoxins in patients with chronic fatigue syndrome. Toxins, 5(4), 605–617. https://doi.org/10.3390/toxins5040605
- Hope, J. (2013). A Review of the Mechanism of Injury and Treatment Approaches for Illness Resulting from Exposure to Water-Damaged Buildings, Mold, and Mycotoxins. The Scientific World Journal, 2013, 767482. https://doi.org/10.1155/2013/76748
- Shoemaker, R.C., House, D.E., & Ryan, J.C. (2013). Vasoactive intestinal polypeptide (VIP) corrects chronic inflammatory response syndrome (CIRS) acquired following exposure to water-damaged buildings. Health, 5(3) 2013, 396-401. https://doi.org/10.4236/health.2013.53053
- Ryan, J.C., Wu, Q., & Shoemaker, R.C. (2015). Transcriptomic signatures in whole blood of patients who acquire a chronic inflammatory response syndrome (CIRS) following an exposure to the marine toxin ciguatoxin. BMC med genomics, (8)15. https://doi.org/10.1186/s12920-015-0089-x
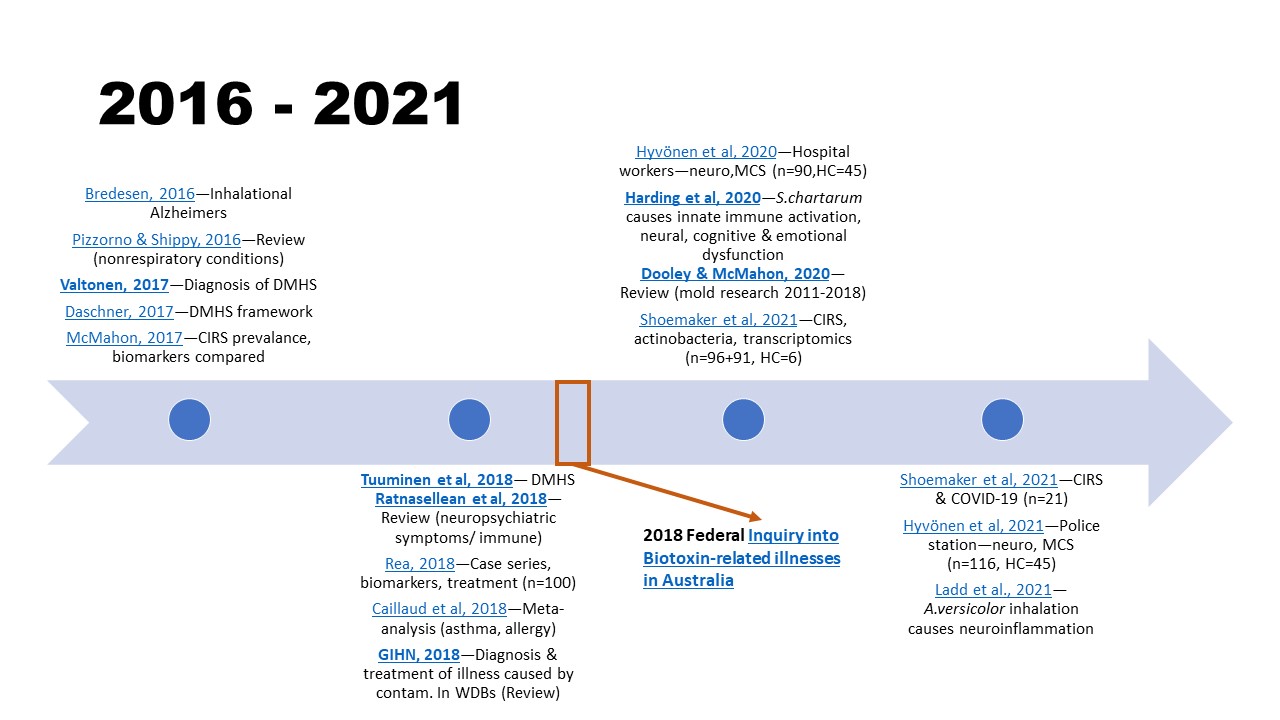
2016 – 2021
- Bredesen D. E. (2016). Inhalational Alzheimer’s disease: an unrecognized – and treatable – epidemic. Aging, 8(2), 304–313. https://doi.org/10.18632/aging.100896
- Pizzorno, J., & Shippy, A. (2016). Is Mold Toxicity Really a Problem for Our Patients? Part 2-Nonrespiratory Conditions. Integrative medicine (Encinitas, Calif.), 15(3), 8–14. PMC4982651
- Daschner A. (2017). An Evolutionary-Based Framework for Analyzing Mold and Dampness-Associated Symptoms in DMHS. Frontiers in immunology, 7, 672. https://doi.org/10.3389/fimmu.2016.00672
- Valtonen V. (2017). Clinical Diagnosis of the Dampness and Mold Hypersensitivity Syndrome: Review of the Literature and Suggested Diagnostic Criteria. Frontiers in immunology, 8, 951. https://doi.org/10.3389/fimmu.2017.00951
- McMahon, S. (2017). An Evaluation of Alternate Means to Diagnose Chronic Inflammatory Response Syndrome and Determine Prevalence. Medical research archives, 5(3), March 2017. https://doi.org/10.18103/mra.v5i3.1125
- Tuuminen, T., & Rinne, K. S. (2017). Severe Sequelae to Mold-Related Illness as Demonstrated in Two Finnish Cohorts. Frontiers in immunology, 8, 382. https://doi.org/10.3389/fimmu.2017.00382
- Ratnaseelan, A. M., Tsilioni, I., & Theoharides, T. C. (2018). Effects of Mycotoxins on Neuropsychiatric Symptoms and Immune Processes. Clinical therapeutics, 40(6), 903–917. https://doi.org/10.1016/j.clinthera.2018.05.004
- Rea W. J. (2018). A Large Case-series of Successful Treatment of Patients Exposed to Mold and Mycotoxin. Clinical therapeutics, 40(6), 889–893. https://doi.org/10.1016/j.clinthera.2018.05.003
- Caillaud, D., Leynaert, B., Keirsbulck, M., Nadif, R., & mould ANSES working group (2018). Indoor mould exposure, asthma and rhinitis: findings from systematic reviews and recent longitudinal studies. European respiratory review, 27(148), 170137. https://doi.org/10.1183/16000617.0137-2017
- Global indoor health network (GIHN). (2018). Diagnosis and Treatment of Illness Caused by Contaminants in Water-Damaged Buildings. www.globalindoorhealthnetwork.com (PDF)
- The Standing Committee on Health, Aged Care and Sport. (2018). Report on the Inquiry into Biotoxin-related Illnesses in Australia. aph.gov.au
- Hyvönen, S., Lohi, J., & Tuuminen, T. (2020). Moist and Mold Exposure is Associated With High Prevalence of Neurological Symptoms and MCS in a Finnish Hospital Workers Cohort. Safety and Health at Work, 11(2), 173–177. https://doi.org/10.1016/j.shaw.2020.01.003
- Harding, C. F., Pytte, C. L., Page, K. G., Ryberg, K. J., Normand, E., Remigio, G. J., DeStefano, R. A., Morris, D. B., Voronina, J., Lopez, A., Stalbow, L. A., Williams, E. P., & Abreu, N. (2020). Mold inhalation causes innate immune activation, neural, cognitive and emotional dysfunction. Brain, Behavior, and Immunity, 87, 218–228. https://doi.org/10.1016/j.bbi.2019.11.006
- Dooley, M. & McMahon, S.W. (2020). A comprehensive review of mold research literature from 2011 – 2018. Internal medicine review, 6(1). http://dx.doi.org/10.18103/imr.v6i1.836
- Shoemaker, R., Neil, V., Heyman, A., van der Westhuizen, McMahon, S., & Lark, D. (2021). Newer molecular methods bring new Insights into human- and building health risk assessments from water-damaged buildings: defining exposure and reactivity, the two sides of causation of CIRS-WDB Illness. Medical Research Archives. 9(3). 1-36. https://doi.org/10.18103/mra.v9i3.2358
- Shoemaker R., McMahon S, Heyman, A., Lark, D, van der Westhuizen, M., & Ryan, J. (2021).Treatable metabolic and inflammatory abnormalities in Post COVID Syndrome (PCS) define the transcriptomic basis for persistent symptoms: Lessons from CIRS. Medical research archives, 9(7). https://doi.org/10.18103/mra.v9i7.2493
- Hyvönen, S., Poussa, T., Lohi, J., & Tuuminen, T. (2021). High prevalence of neurological sequelae and multiple chemical sensitivity among occupants of a Finnish police station damaged by dampness microbiota. Archives of environmental & occupational health, 76(3), 145–151. https://doi.org/10.1080/19338244.2020.1781034
- Ladd, T. B., Johnson, J. A., Jr, Mumaw, C. L., Greve, H. J., Xuei, X., Simpson, E., Barnes, M. A., Green, B. J., Croston, T. L., Ahmed, C., Lemons, A., Beezhold, D. H., & Block, M. L. (2021). Aspergillus versicolor Inhalation Triggers Neuroimmune, Glial, and Neuropeptide Transcriptional Changes. ASN neuro, 13, 17590914211019886. https://doi.org/10.1177/17590914211019886




[…] More reading HERE […]