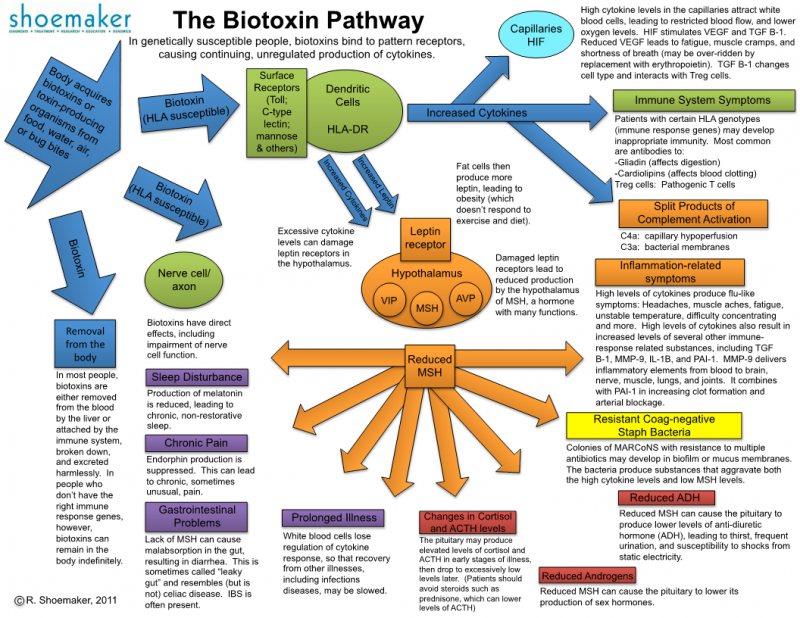
Chronic Inflammatory Response Syndrome (CIRS) is a multi-system, multi-symptom illness caused by inhaling biotoxins and inflammagens produced by micro-organisms such as mould, bacteria, and actinomycetes found in water-damaged buildings (WDB). CIRS, when caused by a water-damaged building, is more commonly known as Mould Illness (Mold Illness, US spelling). However, tick-borne infections such as Borrelia (Lyme disease) and Babesia, toxigenic blue-green algae (cyanobacteria), and certain dinoflagellates (associated with ciguatoxin in reef fish) can also produce biotoxins and potentially cause CIRS.[1]
PDF version (in academic format): https://tinyurl.com/TMSA-CIRS-explained
Can inhaling mould actually harm people?
In the right circumstances, yes.
Science has long recognised the dangers of eating mouldy food. Mycotoxins are the biotoxins produced by certain moulds, some of which can be so toxic to humans as to pose serious health risks and even cause death.[2] Food standards include limits on mycotoxin contamination in grains and other foodstuffs for this reason.
However, there has been far less recognition of how mould and the mycotoxins they form can cause illness when inhaled. Some people view all mould as harmless to humans in this context, and it’s true that most species are. After all, mould spores and their fragments can be found almost everywhere on the planet and we are constantly exposed to them.
The situation is similar with bacteria, which are ubiquitous, too. Usually, our bodies cope with bacterial exposure and some species of bacteria are even healthy for us and make up part of our gut’s microbiome. But in the right circumstances, they can make us sick, for which antibiotics are one possible treatment.
As the Swiss physician Paracelsus famously said: “The dose makes the poison.” In a water-damaged building, a phenomenon called “amplification” occurs whereby certain species of mould and other microbial agents that are more toxigenic flourish and have the resources to produce significantly more biotoxins.
When these biotoxins and other microbial by-products are inhaled over many days and weeks in such an environment, genetically susceptible individuals can become ill with CIRS. Such individuals are highly reactive to damp and mouldy environments, similar to an allergic reaction.
While allergies to mould do exist, CIRS is not technically an allergic response, nor is it a fungal infection, as can also occur. Neither is it purely a toxic response as might be presumed given the exposure to biotoxins, although there can be a toxic component of the illness.
Rather, CIRS is characterised primarily by an over-response of the innate immune system. Inflammation is a natural part of the body’s response to pathogens and can be helpful in the short term. However, when an individual’s immune system is able to detect but not remove biotoxins from the body, the body stays in an inflamed state that only worsens, causing the so-called “chronic inflammatory response” that CIRS is named for.
What constitutes a water-damaged building?
While the scholarly literature uses the term “water-damaged building”, this can seem misleading, suggesting the house has had a significant flooding event such as a bath overflowing or a roof leak. However, high levels of moisture are what drives microbial growth. This means a poorly designed bathroom, condensation forming within the building structure due to flawed design, or even the subfloor area of a building exposed to saturated ground conditions can all be enough to cause unsafe conditions.
The harmful microbial soup found in water-damaged buildings includes mould fragments, mycotoxins, mannans and beta-glucans from mould, endotoxins and exotoxins from bacteria (including gram-positive and gram-negative bacteria, mycobacteria, and actinomycetes), volatile organic compounds (VOCs) from building materials broken down through microbial activity, and microbial VOCs (mVOCs) produced directly by bacteria and mould. Mould is just the most visible, most researched, and easiest microbe to test for.
What is the scientific evidence for CIRS?
There are four major mechanisms for how mould and other microbes associated with dampness can adversely affect human health:[3]
- allergic;
- infection (mycosis) and colonisation;
- toxicity (poisoning); and
- innate immune activation.
CIRS is primarily concerned with the last mechanism, also the least accepted by mainstream medicine. Accepting it means accepting that a major class of pathogen (inhaled biotoxins and associated microbial by-products) has been substantially overlooked in its potential for harm.
Three relevant questions are examined here:
- What is the evidence for causality of dampness and mould causing health problems via innate immune activation?
- What is the current level of understanding of the mechanisms of harm caused by this innate immune activation and related effects?
- Finally, what is the evidence for treatment?
In terms of causality and the mechanisms of harm, the level of evidence has grown significantly stronger on the adverse effects of dampness and mould over the last decade. A recent review of the academic literature found 114 studies between 2011–2018 that associated “chronic indoor microbial growth/dampness exposure with adverse human health effects”.[4] Of these, 112 (98.2%) were supportive in linking chronic exposure to these conditions with altered human health, with effects seen in respiratory, neurological, immunologic (allergic and non-IgE mediated), cognitive, ophthalmologic, and dermatologic systems.
More specifically to the question of innate immune activation and inflammatory responses, the World Health Organisation (WHO), in a 2009 review of previous scientific studies on the effects of dampness and mould, concluded that “Many dampness-associated conditions are likely to involve inflammation, as inflammatory responses to many microbiological agents have been found.”[5]
The same review also noted that “synergistic interactions among microbial agents” can lead to interactions with “unexpected responses, even at low concentrations of microbial (or chemical) agents, so that it is difficult to detect and implicate specific exposures in the causation of damp building-associated adverse health effects.”
They also noted that “Mechanisms of injury include exposure to β-glucans, toxins, spores, cell fragments and chemicals followed by immune stimulation, suppression and autoimmunity as well as neurotoxic effects.”
Later research has shown that the combination of moulds, bacteria, and even dust particles activate stronger, synergistic responses in the immune system than the sum of the effects of individual stimuli.[6] More than just the biotoxins, studies have shown that even spores devoid of toxins can provoke an immune response and inflammation,[7] along with pattern-recognition receptors that recognise fungal cell walls and fungal RNA/DNA.[8]
Moreover, nerve fibres in the nasal cavity provide a pathway to the central nervous system with inhalational exposure that “bypasses the blood–brain barrier”.[9]
A notable study by Kaye Kilburn in 2009 quantitatively measured the effects of mould exposure on multiple physiological systems.[10] This study compared 105 mould-exposed individuals to 100 individuals previously exposed to a variety of chemicals along with 202 unexposed controls. Kilburn found highly significant abnormalities in the mould-exposed individuals on 12 of 14 physiological functions and 10 of 13 psychological tests. Problems included balance issues, slower reactions, lengthened blink-reflex latencies, impaired colour vision and visual fields, decreased grip strength, reduced verbal recall and impaired memory, slowed performance on problem-solving tasks as well as a variety of respiratory problems.
A subsequent 2018 review examined 16 studies (including Kilburn’s) of mould-exposed individuals and found compelling evidence for serious multi-system health effects.[11] As well as more rigorous clinical trials, numerous case studies have been recorded in the academic literature. An early and well-cited example involved researchers discovering an airborne outbreak of toxicosis from trichothecenes (from Stachybotrys chartarum) in a Chicago house that was affecting a family (including their maid) until remediation of the mould contamination.[12]
A 2013 review by Janette Hope listed oxidative stress as a significant mechanism, along with disorders that include: “infections and mycoses, chronic and fungal rhinosinusitis, IgE-mediated sensitivity and asthma, other hypersensitivity reactions, pulmonary inflammatory disease, immune suppression and modulation, autoimmune disorders, mitochondrial toxicity, carcinogenicity, renal toxicity, neurotoxicity, and DNA adducts to nuclear and mitochondrial DNA causing mutations.”[13] Affected individuals might also develop a sensitivity to other chemicals, and there are early clinical reports of electromagnetic sensitivity, too.[14]
Other symptoms from these aforementioned reviews not already mentioned include wheezing, and bronchitis, as well as fatigue, musculoskeletal pain (myalgia), weakness, headaches, gastrointestinal problems, insomnia, dizziness, tremors, palpitations, and mood disorders (e.g., depression and anxiety).
Despite the WHO having acknowledged the fundamental link between dampness, mould, water-damaged buildings and chronic inflammatory and immune effects, a small minority of researchers still contest the issue and consider “mould illness” and other adverse effects to be merely hysteria or the “nocebo” effect.[15] This has also remained the predominant view among many doctors.
In contrast, the evidence for treatment is lacking at present. Predominantly, a single team in the U.S. led by Dr Ritchie Shoemaker have developed the most complete protocol for treatment over the past 23 years with over 20 peer-reviewed papers and following treatment of over 10,000 patients.[16]
Following a pfiesteria outbreak in several waterways in Maryland, Dr Shoemaker discovered that the use of Cholestyramine, a sequestrant normally used for binding cholesterol, helped in the treatment of individuals who displayed learning and memory difficulties following exposure to the pfiesteria toxin.[17],[18],[19]
When he noticed that some individuals living in mouldy houses presented with similar symptoms and also responded to cholestyramine, he began research to understand this related biotoxin illness. However, patients should note that many of his studies are small in scale, some have imperfect methodologies, and a few are published in questionable unranked journals.
Despite this, the Shoemaker Protocol remains the most evidence-based treatment protocol available, the most systematic in identifying the associated biological abnormalities and correcting for them, and the only treatment protocol that has both identified a means of detecting the subtle brain damage found in CIRS patients along with a means for correcting it.[20]
Recent studies by other teams now offer a number of other therapies that might also be helpful in addition to the Shoemaker Protocol. For example, treatment for fungal colonisation is also becoming an increasing part of CIRS protocols, for which reasonable evidence exists.[21]
Dr Shoemaker also coined chronic inflammatory response syndrome as the name for this illness, although several generations of researchers and doctors have investigated mould illness under different nomenclatures: mixed mold mycotoxicosis (MMT), indoor mold sensitivity, sick-building syndrome (SBS), damp building-related illnesses (DBRI), biotoxin-related illnesses, toxic mold syndrome, toxicant-induced loss of tolerance (TILT), dampness and mold hypersensitivity syndrome (DMHS), and environmentally acquired illness (EAI).[22]
More details of treatment are explained under How is CIRS diagnosed and treated?
What symptoms does CIRS cause?
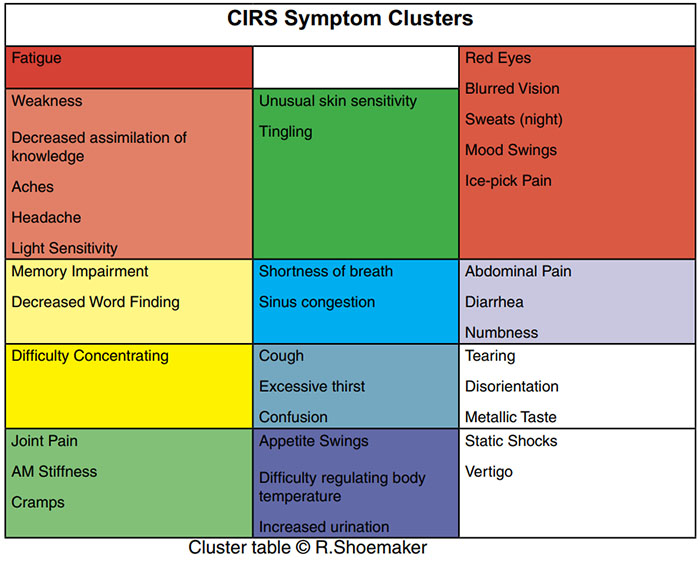
While not a comprehensive list of symptoms, the above table represents research by Dr Ritchie Shoemaker, who found that 35 common symptoms could be categorised into 13 clusters.[23] His clinical research suggested that if a patient possessed eight-or-more clusters of symptoms, the likelihood of CIRS exceeds 95%. A cluster is positive if a patient has one-or-more symptoms in each group.
The multitude of symptoms is partly due to the presence of the immune system throughout the entire body. In a healthy individual, biotoxins will be removed from the blood by the liver or attached to by the adaptive immune system, broken down into harmless adducts, and excreted. In those whose immune systems cannot do this, however, biotoxins can remain in the body indefinitely, continuing to trigger the innate immune system.
This results in chaotic and ineffective inflammatory cascade, which only worsens with continuing exposure to water-damaged environments.
Eventually, the levels of many regulatory hormones are lowered, along with an increase in inflammatory cytokines, dysregulation of gene expression, and even atrophy and inflammation in the brain. Notably, CIRS has been described as the “brain on fire”.[24] The many neuroinflammatory markers associated with CIRS are not just associated in the scientific literature with anxiety and depression[25] but also suicide.[26] Several studies even concluded “neurologists could not differentiate between people with repeated exposure to moldy buildings and people with mild to moderate traumatic brain injury—they had similar neurological and cognitive deficits.”7
Worryingly, a study by Dr Dale Bredesen, a prominent neurodegenerative researcher, suggested that 10% of Alzheimer’s Disease cases are late-stage CIRS patients.[27]
Other components of the illness include the sudden reactivity that many CIRS patients experience to contaminated rooms, or even to bedding, clothing, and other possessions, which is partly mediated by mast cells granulating in response and releasing histamine and pro-inflammatory cytokines.[28]
Given the nature of an illness that can affect potentially every occupant of a “sick building”, entire families can become ill. Moreover, several preliminary studies have also suggested adverse effects on the cognitive development of children.[29],[30]
Finally, CIRS is a frightening diagnosis that involves brain damage; along with a high degree of reactivity to the environment; having perhaps to move house or give away contaminated possessions; while dealing with a medical system, family, and friends who have not necessarily heard of or believe in this illness; combined with the loss of income while ill; suffering from neuropsychiatric symptoms due to an inflamed brain; all the while battling many physical symptoms including severe fatigue. This is more than anyone’s fair share of adversity.
CIRS is a highly traumatic illness to endure, one which often takes 18 months or longer to fully recover from, and patients need a strong support network.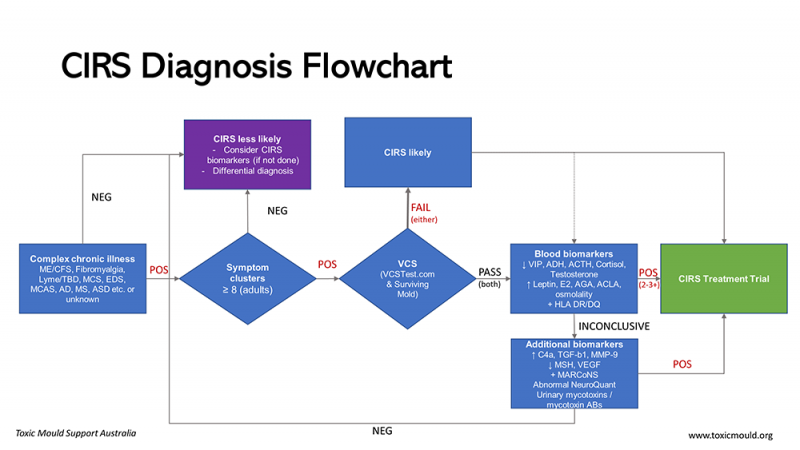
How is CIRS diagnosed?
The current diagnostic criteria for CIRS are as follows:
- laboratory abnormalities similar to those seen in published peer-reviewed studies;
- multiple symptoms involving multiple systems (CIRS symptom clusters); and
- potential of exposure to a water-damaged building with amplified microbial growth, as detected by the presence of visible mould, water damage, musty odours, or commercial testing.
The laboratory abnormalities include innate immune and inflammatory biomarkers, regulatory hormones, and markers of genetic susceptibility:[31]
- deficits in visual contrast sensitivity (VCS); and
- biotoxin-susceptible HLA DR-DQ haplotypes;[32]
- elevated transforming growth factor beta (TGF-β1), C4a (complement), and matrix metalloproteinase 9 (MMP-9); and
- low vascular endothelial growth factor (VEGF), alpha melanocyte stimulating hormone (α-MSH), and vasoactive intestinal polypeptide (VIP).
- Volumetric MRI test for microscopic interstitial oedema/neuroinflammation and atrophy/neuronal loss in a signature pattern.
This last test uses computer software to accurately measure the volumes of different regions of the brain. While a regular MRI might show as normal for a CIRS patient, the volumetric MRI can scan for a signature pattern of swelling and atrophy in specific regions of the brain that is characteristic of CIRS. This allows for the condition to be diagnosed early before the damage becomes more pronounced.
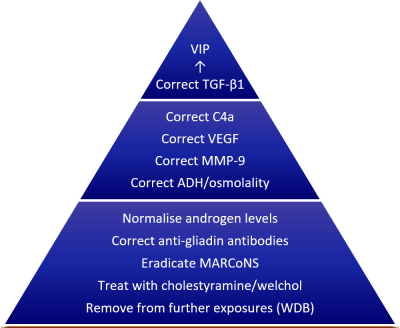
How is CIRS Treated?
Treatment always starts with the removal of the patient from further exposure to any water-damaged buildings, such as their home, workplace, or school building. Next, the patient takes sequestrants such as Cholestyramine (CSM) or Welchol, which bind with biotoxins that are recirculated via the bile acids. These first two steps alone can have a significant effect on correcting the patient’s inflammatory markers. (However, CSM and Welchol can cause a short-term intensification of symptoms due to allowing some biotoxins to re-enter the bloodstream instead of cell receptors, causing a temporary increase in inflammation.) Some practitioners also use non-pharmaceutical options such as bentonite clay, activated charcoal, and chitosan, depending on the results of urinary mycotoxin testing.[33]
Shoemaker Protocol (© R. Shoemaker)
Practitioners will prescribe a variety of medications and supplements to correct the other abnormalities. For example, Multiple Antibiotic Resistant Coagulase Negative Staphylococci (MARCoNS) are bacteria that colonise the sinuses in many CIRS patients, forming biofilms and creating exotoxins. Treating the MARCoNS infection often involves nasal sprays to break down bacterial biofilms and kill the embedded bacteria.
The final treatment is usually another nasal spray of a bioidentical hormone: Vasoactive Intestinal Polypeptide. This neurotransmitter peptide in the brain is usually low in CIRS patients. The nasal spray is used for at least several months and has profound effects, such as:20
- increased plasma VIP levels;
- reduced inflammatory cytokines (TGF-β1, C4a, MMP-9);
- increased vitamin-D levels;
- normalised low testosterone levels in males; and
- reduced symptoms to the level of healthy controls.
Most importantly, the characteristic signature of swelling and atrophy in the brain can sometimes be completely reversed to normal. Many patients report greatly increased quality of life following this stage of treatment, and a complete recovery is often possible.[34]
What are common misdiagnoses of CIRS?
Biotoxin exposure suppresses the immune system. Clinicians and patients have routinely noted that CIRS may be an underlying cause or a co-factor in:[35]
- chronic fatigue syndrome (CFS) / myalgic encephalomyelitis (ME);
- fibromyalgia;
- multiple sclerosis;
- somatisation (i.e., hypochondria);
- attention deficit hyperactivity disorder (ADD/ADHD);
- depression, stress, and anxiety;
- allergies;
- irritable bowel syndrome (IBS);
- post-traumatic stress disorder (PTSD); and
- other autoimmune disorders.
In seeking diagnosis, patients are recommended to investigate and exclude other diagnoses.
Which doctors treat CIRS?
As of 2020, only a small number of registered GPs in Australia have the knowledge and experience necessary to diagnose and treat CIRS. Most are associated with the International Society for Environmentally Acquired Illnesses (ISEAI).[36]
A list of practitioners (by state) is kept updated on the TMSA website at the following link:
CIRS-Aware Health Professionals
While appointments are partially covered by Medicare, a number of the relevant tests and medications are not covered at this point in time. This is, in part, due to Australia lacking any pathologies that can accurately test some of the relevant immune and inflammatory markers. As such, these blood tests have to be flown to pathologies in the U.S. instead.
Who can inspect my home or workplace for mould?
A qualified specialist called an Indoor Environmental Professional (IEP) is recommended for inspecting a building for mould, bacteria, water damage, and moisture. IEP is an umbrella term for several professions or qualifications including occupational/industrial hygienists, American Council for Accredited Certification (ACAC), building biologists and mycologists/ microbiologists.[37]
IEPs should visually inspect the outside and inside of a building; undertake moisture mapping; use microbial sampling to identify the location, extent, and type of microbes present; and give the client a report of their findings. If the IEP recommends remediation of the building, they can outline a scope of remedial works. Ideally the IEP and mould remediator are separate to prevent conflict of interest.
While systematic tests for measuring microbial growth in buildings have been developed, such as the Environmental Relative Mouldiness Index (ERMI), they are not definitive given that they do not cover all known microbial inflammagens, nor are the synergistic interactions between inflammagens understood, and also given individual responses to different stimuli.[38]
What about contaminated homes and possessions?
Remediating a water-damaged building can be difficult, because while mould and microbial agents can be killed, the biotoxins contaminating the building and possessions are harder to remove. Source removal, rather than just killing, of microbes (and their toxins) is required.
The ABCs of mould remediation are:[39]
- Abate the water intrusion.
- Building materials that are contaminated must be removed (or encapsulated).
- Clean reservoirs on possessions, in the air, and on all surfaces. (Every room must be cleaned if air from one room could get into another.)
Remediation can be expensive and, if done poorly, not necessarily create a healthier environment. Professional remediators should follow the ANSI/IICRC S520 mold remediation standard at a minimum and ideally hold current IICRC certification.
Porous possessions cannot always be cleaned, such as mattresses, and may need to be discarded. An air purifier can improve the air quality in the home, too. Occasionally, if a problematic home cannot be sufficiently remediated, moving to a new house or apartment might be necessary.
The point of remediation is not to live without any mould or bacteria (given the near impossibility of this), but rather to avoid excessive moisture in the building envelope. An open, airy, and dry home will still possess a normal microbial ecology (defined as Level 1 by the IICRC), just one that isn’t harmful.
For those renting, it may be difficult to break the lease on a property due to the lack of acceptance of this illness. The onus will be on tenants to prove the home is unfit for tenancy by providing sufficient evidence of water damage or microbial contamination, a diagnosis of CIRS (or related), and evidence regarding the illness.
How can affected individuals find quality help?
When dealing with any poorly understood chronic illness, patients can easily spend much time and money on poorly proven treatments and services. Science simply does not understand the many manifestations of biotoxin-related illnesses at this time. Even the best treatment protocols for CIRS that have sufficient scholarly evidence for every step do not necessarily lead to a complete recovery for all patients.
Given that the majority of practitioners currently treating CIRS at present also specialise in integrative medicine, treatments can include a greater reliance on supplements and alternative therapies instead of pharmaceuticals. Some of these treatments, such as the use of certain flavonoids for the treatment of mast-cell activation, do possess scholarly evidence.[40]
Other prescribed treatments might be based on preliminary or unpublished clinical evidence. As such, it can be difficult to assess whether a particular treatment possesses merit. Patients’ regular (allopathic) doctors might be able to provide further guidance in this regard.
Some practitioners may even recommend patients try camping in a dry climate with low levels of dampness and mould in order to see if their health improves. A two-week “mould sabbatical” can attune a patient to mould and toxins in their environment. This feedback can inform their decision-making process on where to live and what possessions to save, remediate, or discard.
Why do some websites say CIRS isn’t real?
Frustratingly, a disinformation campaign exists around this illness. Just as the adverse effects of radium, coal, asbestos, and tobacco were denied by corporate and special interests for years, the same is true of mould.
In the early 2000s, a doctor who was previously involved with the cigarette manufacturer Philip Morris to discredit the link between smoking and cancer, and with no expertise in indoor air quality or mould, began publishing studies and reviews that purported to show that levels of inhaled mycotoxins in ordinary settings could never be high enough to cause serious harm.[41] Despite undisclosed conflicts of interest and that the major study he and his colleagues published has been discredited,[42] a review he co-wrote is still being promoted by the largest lobbying group in the U.S.[43] He and other colleagues used this misinformation to testify on behalf of insurance companies in order to deny mould-related insurance and workers’ compensation claims.[44]
This ongoing misconduct has convinced many that the illness couldn’t be real despite a growing body of science.
What is the future for CIRS?
With many of the most compelling studies and reviews on CIRS having been published only in the past decade, many government and medical agencies have not formally recognised CIRS yet. Furthermore, many questions remain unanswered about this illness.
For example, has humanity’s use of fungicides caused certain species to evolve, becoming more harmful to humans than they previously were (similar to antibiotic-resistant bacteria)? Are we seeing interactions between nanoparticles from industrial air pollution and mould spores that wouldn’t have taken place in previous eras?[45] Are newer building materials that mould can grow and feed on causing new mycotoxins to be produced? And what other biological mechanisms, such as T-cell receptors, cause these chronic inflammatory responses in response to dampness and mould?[46]
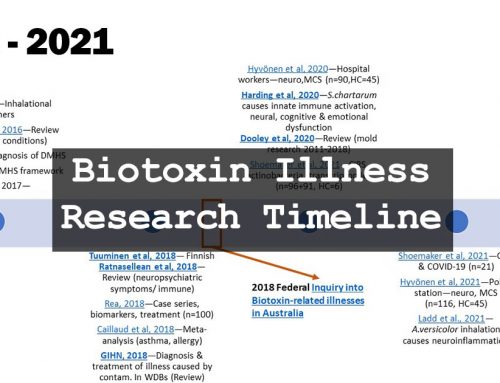
Given the need for further research and greater awareness, Australians can consider themselves quite fortunate in how their country is responding to improve the situation. Following a 2018 Federal Inquiry into Biotoxin-Related Illnesses, the Australian Government recently responded with the steps they are taking to better understand and treat CIRS and related illnesses.[47] In 2019, the National Construction Code was updated with higher standards regarding condensation management in residential buildings. And the National Health and Medical Research Council (NHMRC) are currently designing a targeted call for further research into biotoxin-related illnesses in Australia (and have asked TMSA for their involvement).
With all of this underway and doctors continually working to refine and improve treatment protocols, the prospects for CIRS patients are only improving.
References
[1] Version 1.2 of this explainer published 21 December 2020 by Toxic Mould Support Australia (TMSA). TMSA are the primary support group in Australia and New Zealand for CIRS patients, providing both a Facebook group and a website at toxicmould.org.
[2] Misihairabgwi, J. M., Ezekiel, C. N., Sulyok, M., Shephard, G. S., & Krska, R. (2019). Mycotoxin contamination of foods in Southern Africa: A 10-year review (2007–2016). Critical reviews in food science and nutrition, 59(1), 43–58.
[3] Wikimedia Foundation, Inc. (2020, November 26). Mold health issues. Wikipedia, the free encyclopedia. Retrieved November 29, 2020, from https://en.wikipedia.org/wiki/Mold_health_issues
[4] Dooley, M. & McMahon, S. W. (2020). A comprehensive review of mold research literature from 2011–2018. Internal Medicine Review.
[5] Heseltine, E., & Rosen, J. (Eds.). (2009). WHO guidelines for indoor air quality: dampness and mould. WHO Regional Office Europe.
[6] Morris et al. (2016). The Putative Role of Viruses, Bacteria, and Chronic Fungal Biotoxin Exposure in the Genesis of Intractable Fatigue Accompanied by Cognitive and Physical Disability. Molecular neurobiology, 53(4), 2550–2571.
[7] Harding et al. (2020). Mold inhalation causes innate immune activation, neural, cognitive and emotional dysfunction. Brain, Behavior, and Immunity, 87, 218–228.
[8] Dambuza et al. (2017). Fungal Recognition and Host Defense Mechanisms. Microbiology spectrum, 5(4), 10.1128/microbiolspec.FUNK-0050-2016.
[9] Ammann, H. M. (2016). Inhalation exposure and toxic effects of mycotoxins. In Biology of microfungi (pp. 495–523). Springer, Cham.
[10] Kilburn K. H. (2009). Neurobehavioral and pulmonary impairment in 105 adults with indoor exposure to molds compared to 100 exposed to chemicals. Toxicology and industrial health, 25(9-10), 681–692.
[11] Ratnaseelan et al. (2018). Effects of mycotoxins on neuropsychiatric symptoms and immune processes. Clinical Therapeutics, 40(6), 903–917.
[12] Croft et al. (1986). Airborne outbreak of trichothecene toxicosis. Atmospheric Environment (1967), 20(3), 549–552.
[13] Hope J. (2013). A review of the mechanism of injury and treatment approaches for illness resulting from exposure to water-damaged buildings, mold, and mycotoxins. The Scientific World Journal, 2013.
[14] Tuuminen T. (2020). The Roles of Autoimmunity and Biotoxicosis in Sick Building Syndrome as a “Starting Point” for Irreversible Dampness and Mold Hypersensitivity Syndrome. Antibodies (Basel, Switzerland), 9(2), 26.
[15] Chang, C., & Gershwin, M. E. (2019). The myth of mycotoxins and mold injury. Clinical Reviews in Allergy & Immunology, 57(3), 449-455.
[16] A complete list of Dr Shoemaker’s publications, peer-reviewed and otherwise, can be found at the TMSA website.
[17] Grattan et al. (1998). Learning and memory difficulties after environmental exposure to waterways containing toxin-producing Pfiesteria or Pfiesteria-like dinoflagellates. The Lancet, 352(9127), 532-539.
[18] Shoemaker, R. (1998). Treatment of persistent Pfiesteria-human illness syndrome. Maryland Medical Journal, 47(2), 64.
[19] Shoemaker, R. C. (2001). Residential and recreational acquisition of possible estuary-associated syndrome: a new approach to successful diagnosis and treatment. Environmental Health Perspectives, 109, 791-796.
[20] Shoemaker et al. (2013). Vasoactive intestinal polypeptide (VIP) corrects chronic inflammatory response syndrome (CIRS) acquired following exposure to water-damaged buildings. Health, 5, 396–401.
[21] Brewer, J., Thrasher, J. & Hooper, D. (2013). Chronic illness associated with mold and mycotoxins: is naso-sinus fungal biofilm the culprit? Toxins, 24, 6(1), 66-80.
[22] Tuuminen, T., & Lohi, J. (2018). Immunological and toxicological effects of bad indoor air to cause Dampness and Mold Hypersensitivity Syndrome. AIMS allergy and immunology, 2(4), 190-203.
[23] Shoemaker, R. C., & House, D. E. (2006). Sick building syndrome (SBS) and exposure to water-damaged buildings: Time series study, clinical trial and mechanisms. Neurotoxicology and Teratology, 28(5), 573-588.
[24] Ackerley, M. (2014, March 14). Brain on Fire: The Role of Toxic Mold in Triggering Psychiatric Symptoms. Paradigm Change.
[25] Osimo et al. (2020). Inflammatory markers in depression: A meta-analysis of mean differences and variability in 5,166 patients and 5,083 controls. Brain, Behavior, and Immunity, 87, 901-909.
[26] Isung et al. (2012). Low plasma vascular endothelial growth factor (VEGF) associated with completed suicide. World Journal of Biological Psychiatry, 13(6), 468-473.
[27] Bredesen, D. E. (2016). Inhalational Alzheimer’s disease: An unrecognized—and treatable—epidemic. Aging, 8(2), 304-313.
[28] Kritas et al. (2018). Impact of mold on mast cell-cytokine immune response. Journal of biological regulators and homeostatic agents, 32(4), 763–768.
[29] Casas et al. (2013). Early life exposures to home dampness, pet ownership and farm animal contact and neuropsychological development in 4 year old children: a prospective birth cohort study. International journal of hygiene and environmental health, 216(6), 690–697.
[30] Jedrychowski et al. (2011). Cognitive function of 6-year old children exposed to mold-contaminated homes in early postnatal period. Prospective birth cohort study in Poland. Physiology & behavior, 104(5), 989–995.
[31] Shoemaker et al. (2014). Structural brain abnormalities in patients with inflammatory illness acquired following exposure to water-damaged buildings: A volumetric MRI study using NeuroQuant®. Neurotoxicology and Teratology, 45, 18-26.
[32] Shoemaker, R. C. (2003). Linkage disequilibrium in alleles of HLA DR: differential association with susceptibility to chronic illness following exposure to biologically produced neurotoxins. American Society of Microbiology. (Conference peer review.)
[33] Nathan, N. (2018). Toxic: Heal your body from mold toxicity, Lyme disease, multiple chemical sensitivities, and chronic environmental illness. Victory Belt Publishing.
[34] Shoemaker et al. (2017). Intranasal VIP safely restores volume to multiple grey matter nuclei in patients with CIRS. Internal Medicine Review, 3(4).
[35] Shoemaker, R. C. (2011, March 3). Common misdiagnoses of mold sickness. Surviving Mold.
[36] International Society for Environmentally Acquired Illness. (2020, November 24). Find a professional. ISEAI.
[37] Toxic Mould Support Australia. (2020, November 30). Building inspection and remediation.
[38] Vesper et al. (2007). Development of an environmental relative moldiness index for US homes. Journal of Occupational and Environmental Medicine, 49(8), 829-833.
[39] Shoemaker et al. (2019, November 30). Moldy buildings, CIRS, sick people, and damaged brains: 25 years of research brought us to the cure word (Part 4). Townsend Letter.
[40] Theoharides et al. (2015). Brain “fog,” inflammation and obesity: key aspects of neuropsychiatric disorders improved by luteolin. Frontiers in neuroscience, 9, 225.
[41] Hardin et al. (2003). Adverse human health effects associated with molds in the indoor environment. Journal of Occupational and Environmental medicine, 45(5), 470-478.
[42] Craner, J. (2008). A critique of the ACOEM statement on mold: undisclosed conflicts of interest in the creation of an” evidence-based” statement. International journal of occupational and environmental health, 14(4), 283.
[43] U.S. Chamber Institute for Legal Reform; Center for Legal Policy at The Manhattan Institute. (2013, November 22). The growing hazard of mold litigation. U.S. Chamber of Commerce.
[44] Armstrong, D. (2007, January 10). Amid suits over mold, experts wear two hats. The Wall Street Journal.
[45] Westmeier et al. (2018). Nanoparticle decoration impacts airborne fungal pathobiology. Proceedings of the National Academy of Sciences of the United States of America, 115(27), 7087–7092.
[46] Dennis et al. (2009). Fungal exposure endocrinopathy in sinusitis with growth hormone deficiency: Dennis-Robertson syndrome. Toxicology and Industrial Health, 25(9-10), 669-680.
[47] Commonwealth of Australia. (2020, March 3). Australian Government response to the Inquiry into Biotoxin-related Illnesses in Australia. Parliament of Australia.
[48] Shoemaker, R. C. (2011). The Biotoxin Pathway. Surviving Mold.



You must be logged in to post a comment.